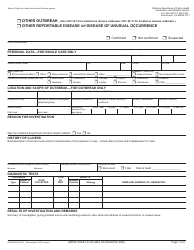
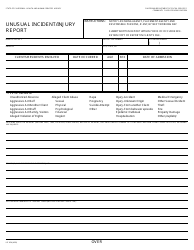
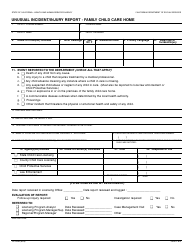
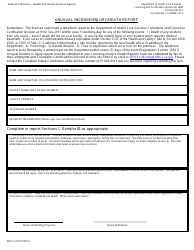
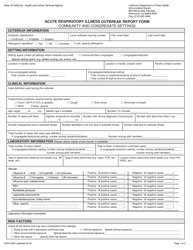
Instructions for Form CDPH8567 Foodborne Disease Outbreak Report - California
This document contains official instructions for Form CDPH8567 , Foodborne Disease Outbreak Report - a form released and collected by the California Department of Public Health. An up-to-date fillable Form CDPH8567 is available for download through this link.
FAQ
Q: What is Form CDPH8567?
A: Form CDPH8567 is a document used to report foodborne disease outbreaks in California.
Q: Who is required to complete Form CDPH8567?
A: Healthcare providers, laboratories, and local health departments are required to complete Form CDPH8567.
Q: What information is needed to complete Form CDPH8567?
A: Form CDPH8567 requires information about the affected individuals, suspected food sources, and symptoms reported.
Q: How should Form CDPH8567 be submitted?
A: Completed Form CDPH8567 should be submitted to the local health department or the California Department of Public Health.
Q: Are there any deadlines for submitting Form CDPH8567?
A: Yes, Form CDPH8567 should be submitted as soon as possible, ideally within 24 hours of identifying a potential foodborne disease outbreak.
Q: What happens after submitting Form CDPH8567?
A: After submitting Form CDPH8567, the local health department or California Department of Public Health will investigate the reported outbreak.
Q: What is the purpose of Form CDPH8567?
A: Form CDPH8567 helps in identifying and investigating foodborne disease outbreaks to protect public health.
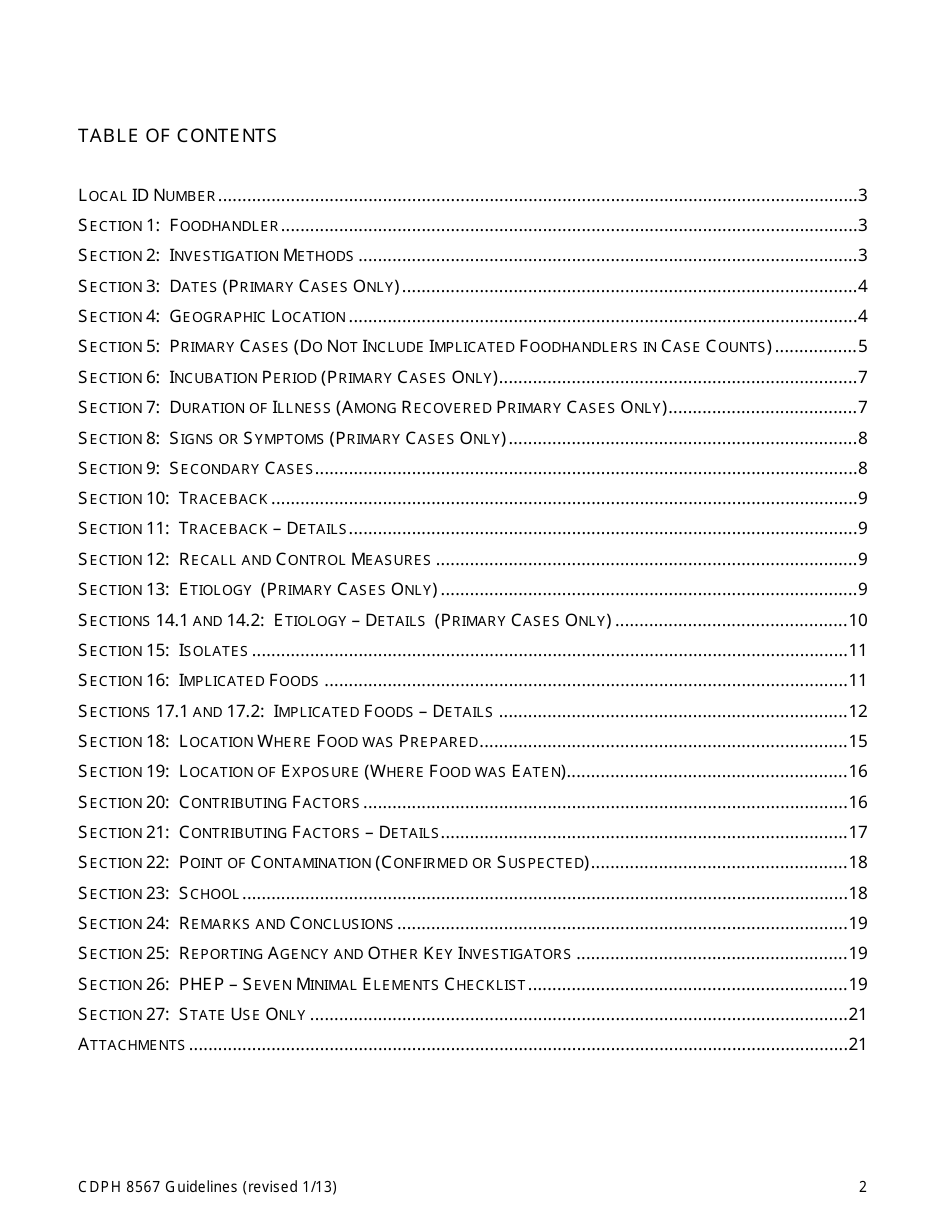
Instruction Details:
- This 21-page document is available for download in PDF;
- Actual and applicable for the current year;
- Complete, printable, and free.
Download your copy of the instructions by clicking the link below or browse hundreds of other forms in our library of forms released by the California Department of Public Health.