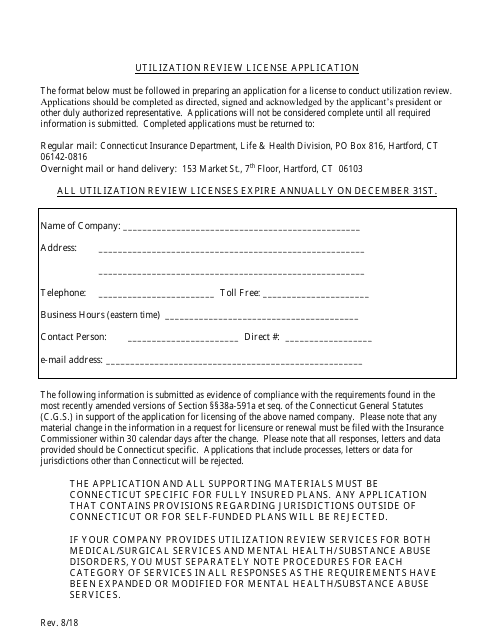
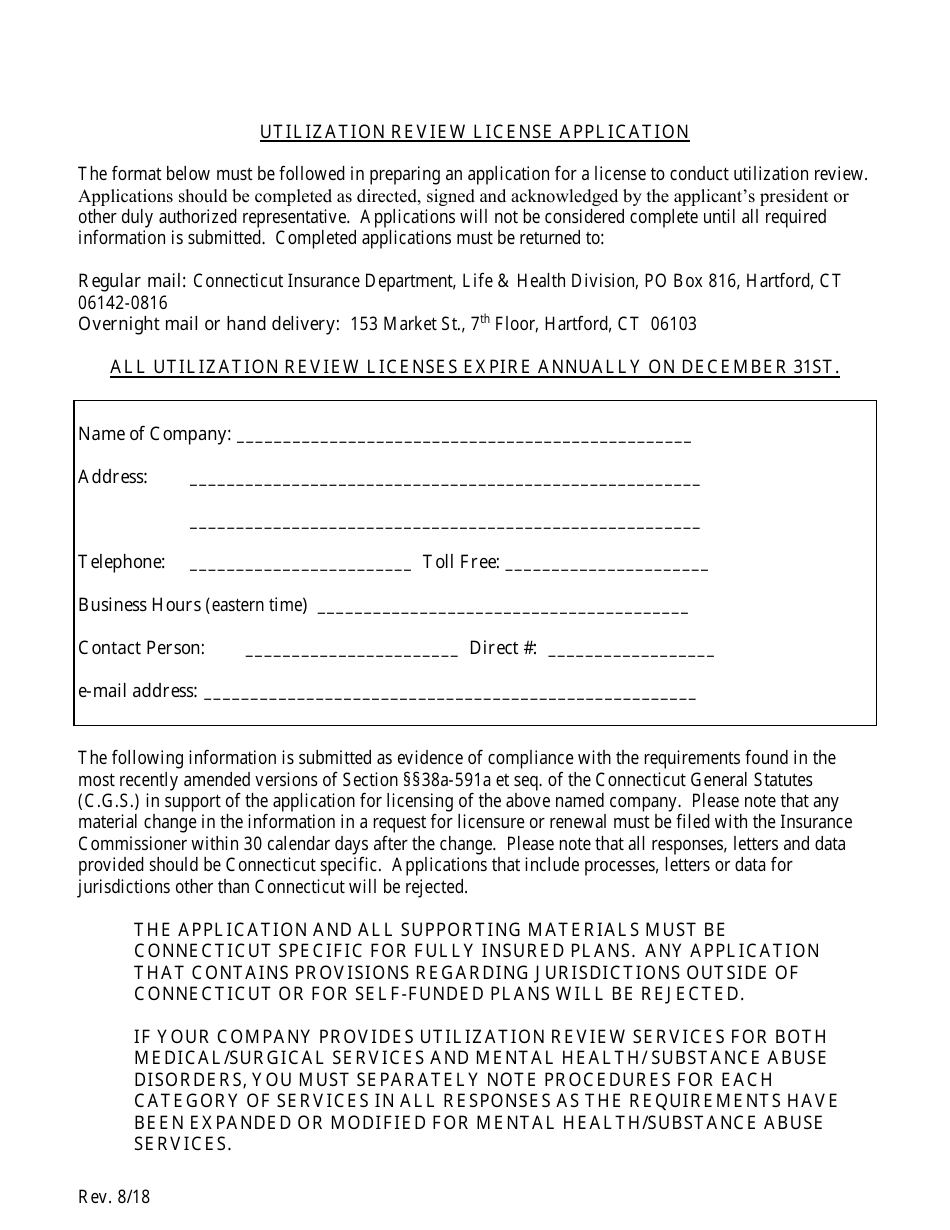
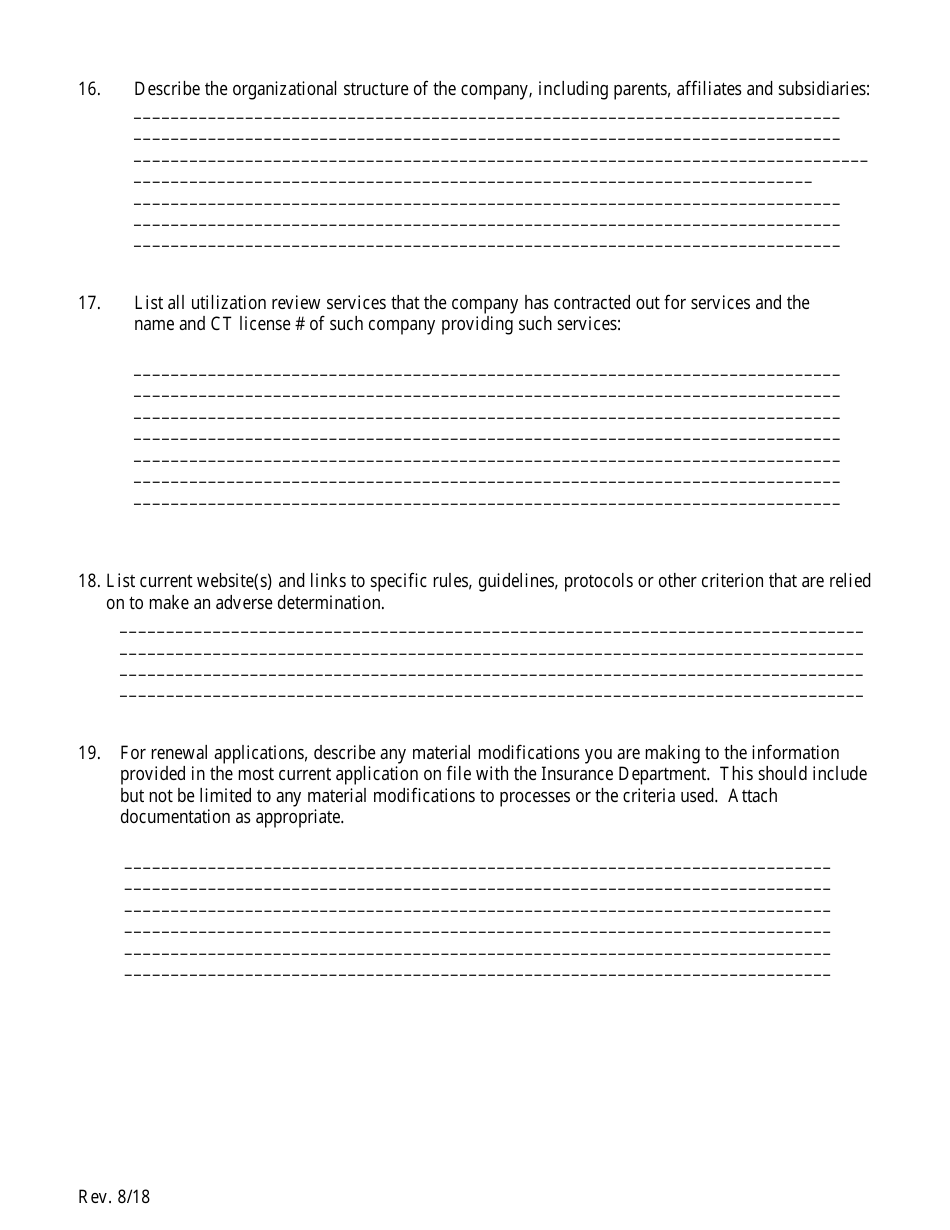
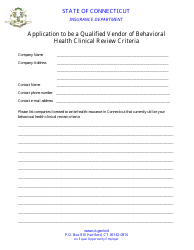
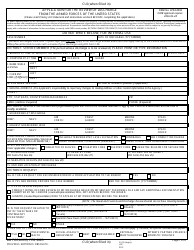
Utilization Review License Application Form - Connecticut
Utilization Review License Application Form is a legal document that was released by the Connecticut Insurance Department - a government authority operating within Connecticut.
FAQ
Q: What is a Utilization Review License?
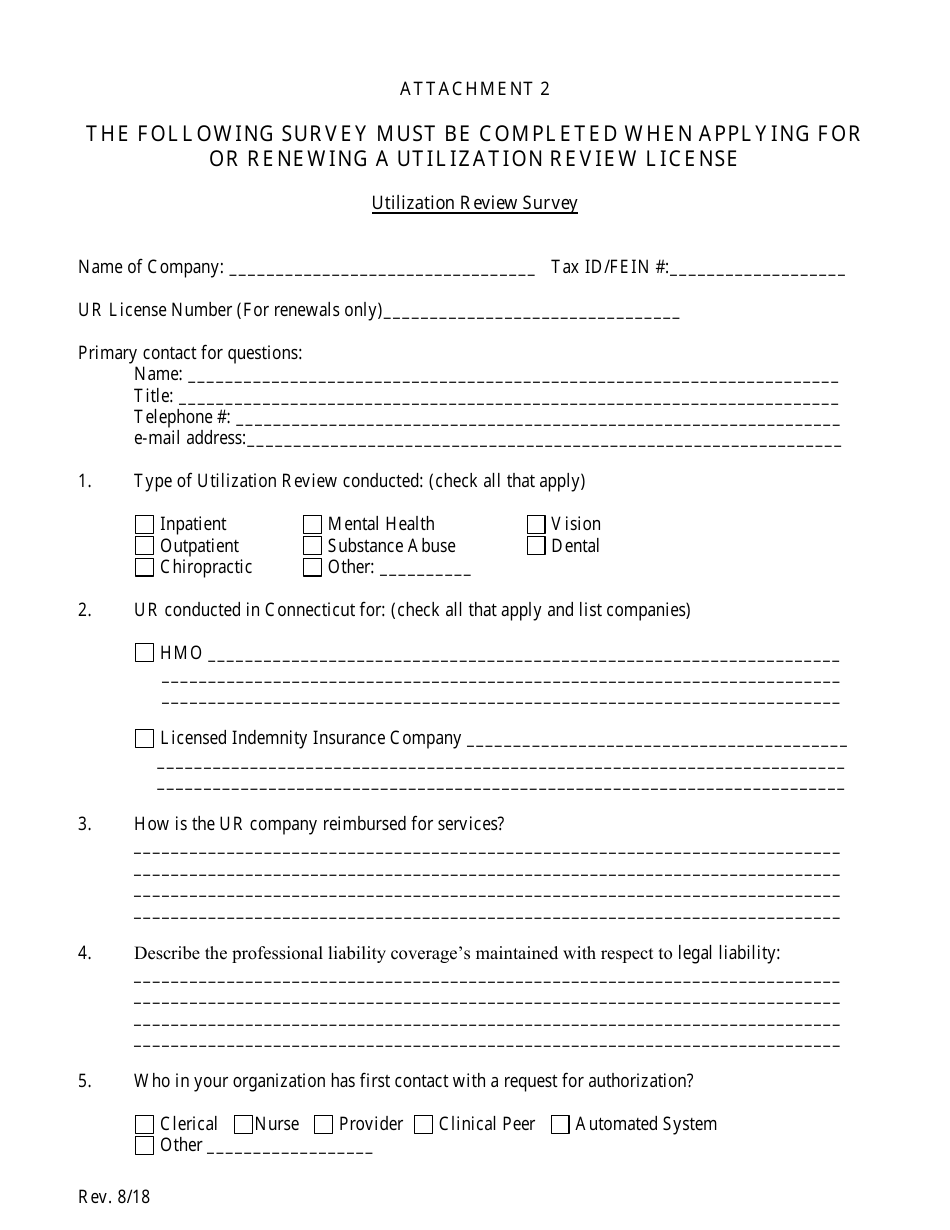
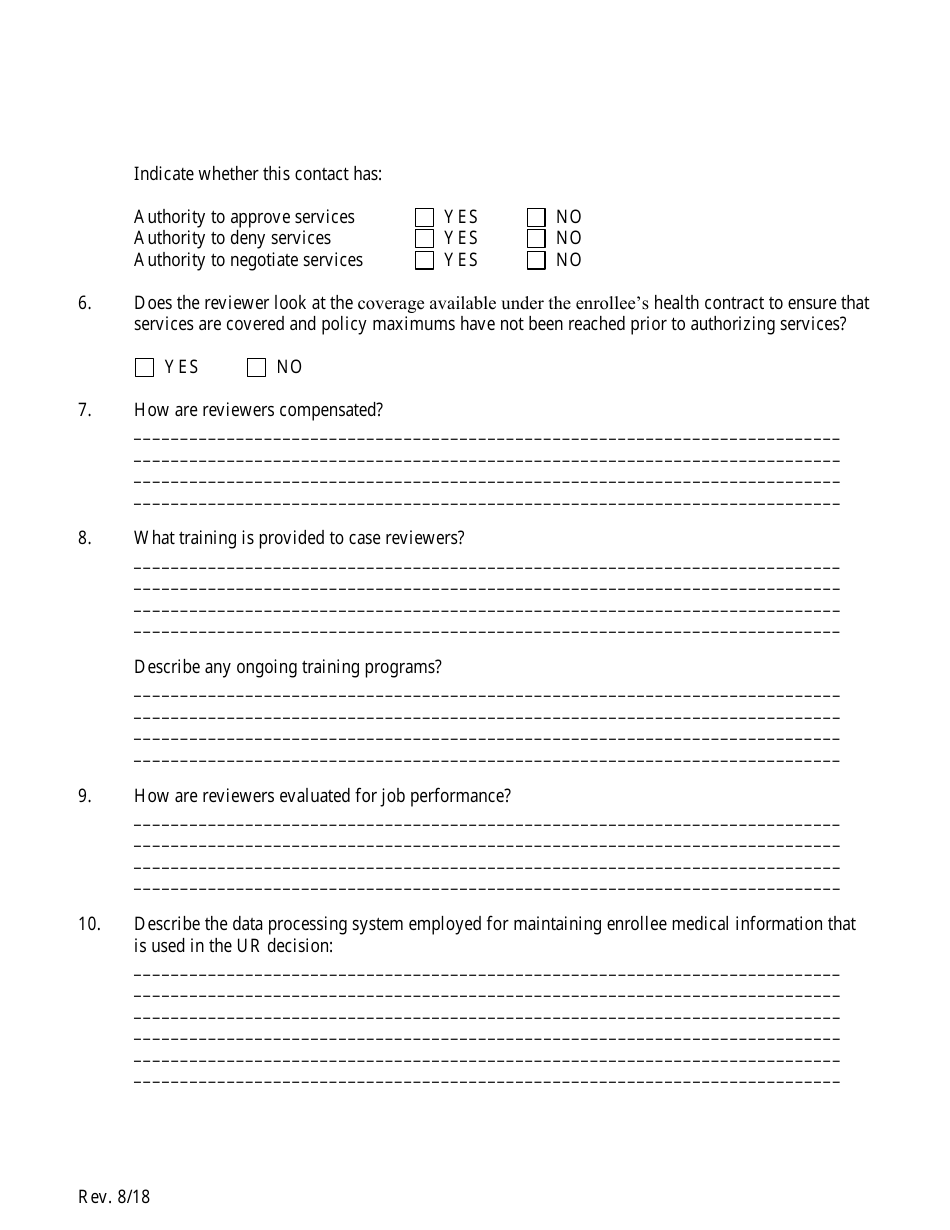
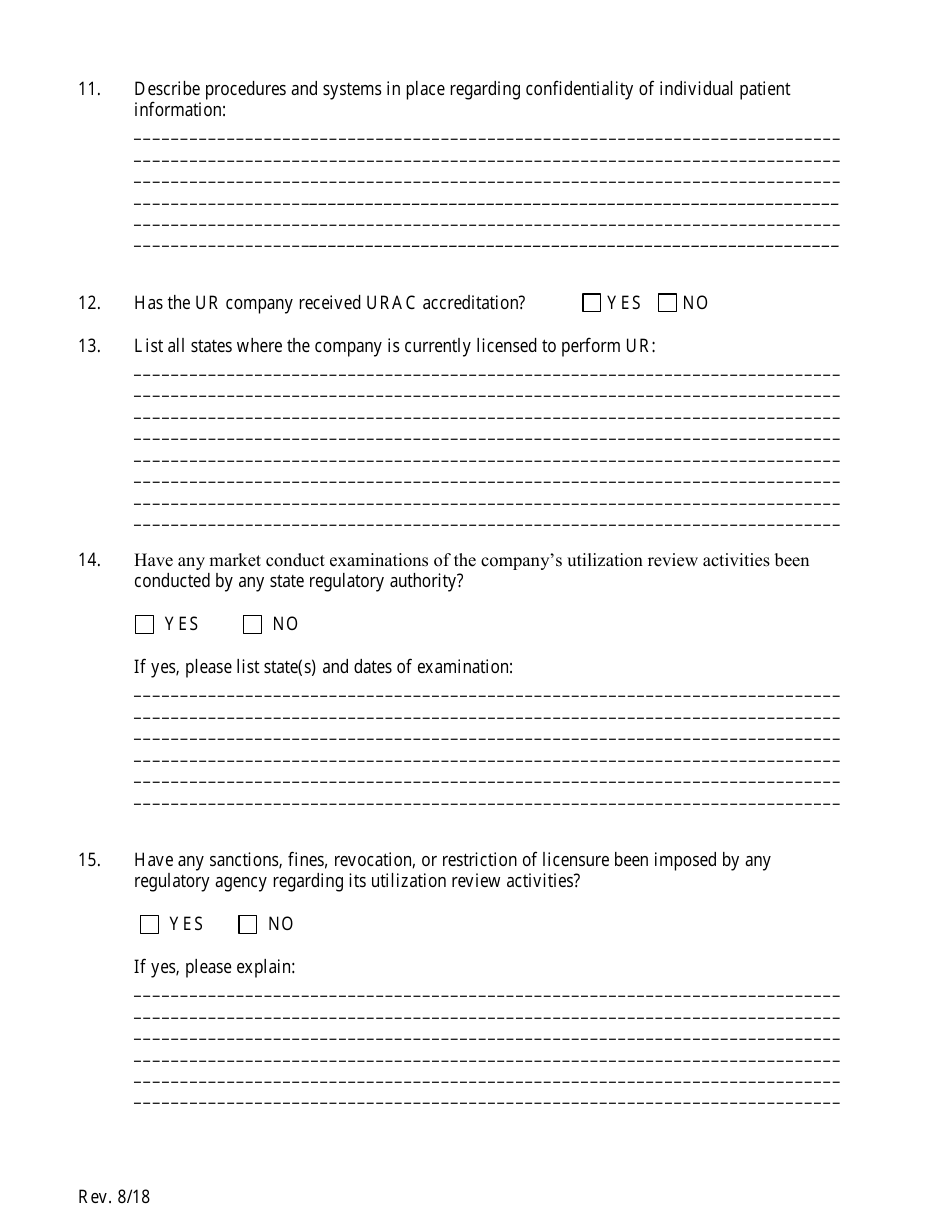
A: A Utilization Review License is a license required by the state of Connecticut for entities that perform utilization review services.
Q: What is utilization review?
A: Utilization review is the process of reviewing medical services and treatments to ensure they are medically necessary and appropriate.
Q: Who needs to apply for a Utilization Review License in Connecticut?
A: Entities that provide utilization review services in Connecticut need to apply for a Utilization Review License.
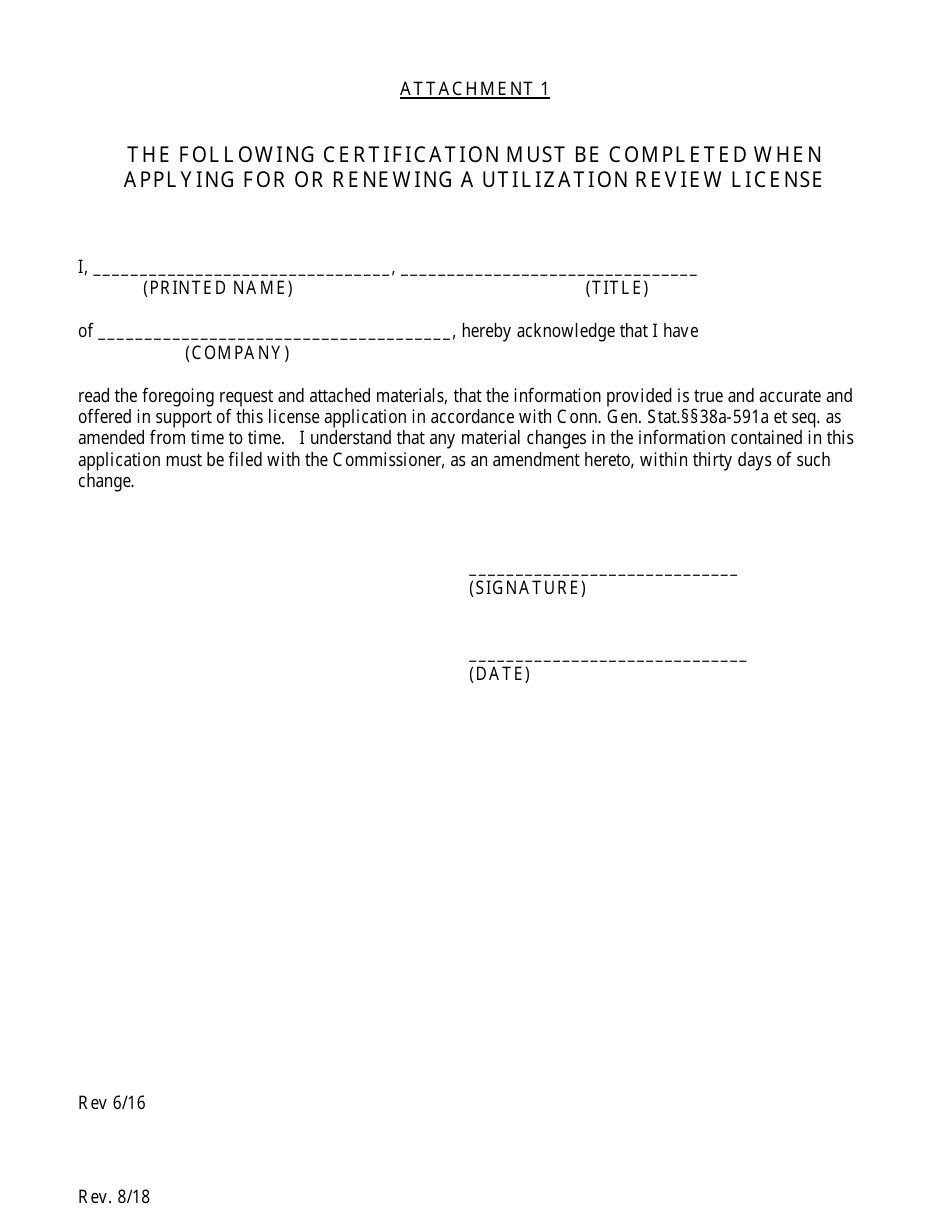
Q: How do I apply for a Utilization Review License in Connecticut?
A: You can apply for a Utilization Review License in Connecticut by completing and submitting the application form provided by the state.
Q: Are there any requirements or qualifications to apply for a Utilization Review License in Connecticut?
A: Yes, there are requirements and qualifications that must be met to apply for a Utilization Review License in Connecticut. These requirements may include proof of financial stability, a designated UR agent, and compliance with state laws and regulations.
Q: How long does it take to process a Utilization Review License application in Connecticut?
A: The processing time for a Utilization Review License application in Connecticut may vary. It is best to check with the Connecticut Department of Public Health for the most up-to-date processing times.
Q: What happens after I submit the Utilization Review License application in Connecticut?
A: After submitting the Utilization Review License application in Connecticut, it will be reviewed by the Connecticut Department of Public Health. They will notify you of their decision.
Q: How long is a Utilization Review License valid in Connecticut?
A: A Utilization Review License in Connecticut is typically valid for one year. It must be renewed annually to remain in compliance with state regulations.
Form Details:
- Released on August 1, 2018;
- The latest edition currently provided by the Connecticut Insurance Department;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Connecticut Insurance Department.