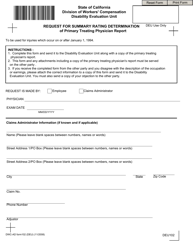
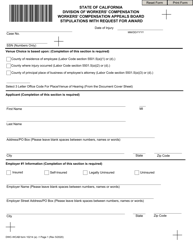
DWC Form RFA Request for Authorization - California
What Is DWC Form RFA?
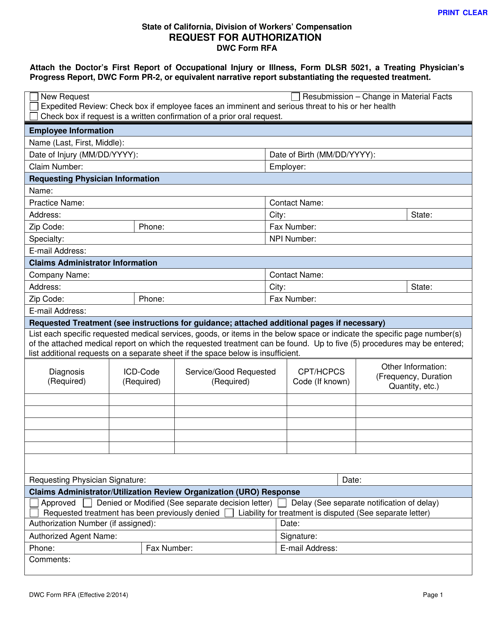
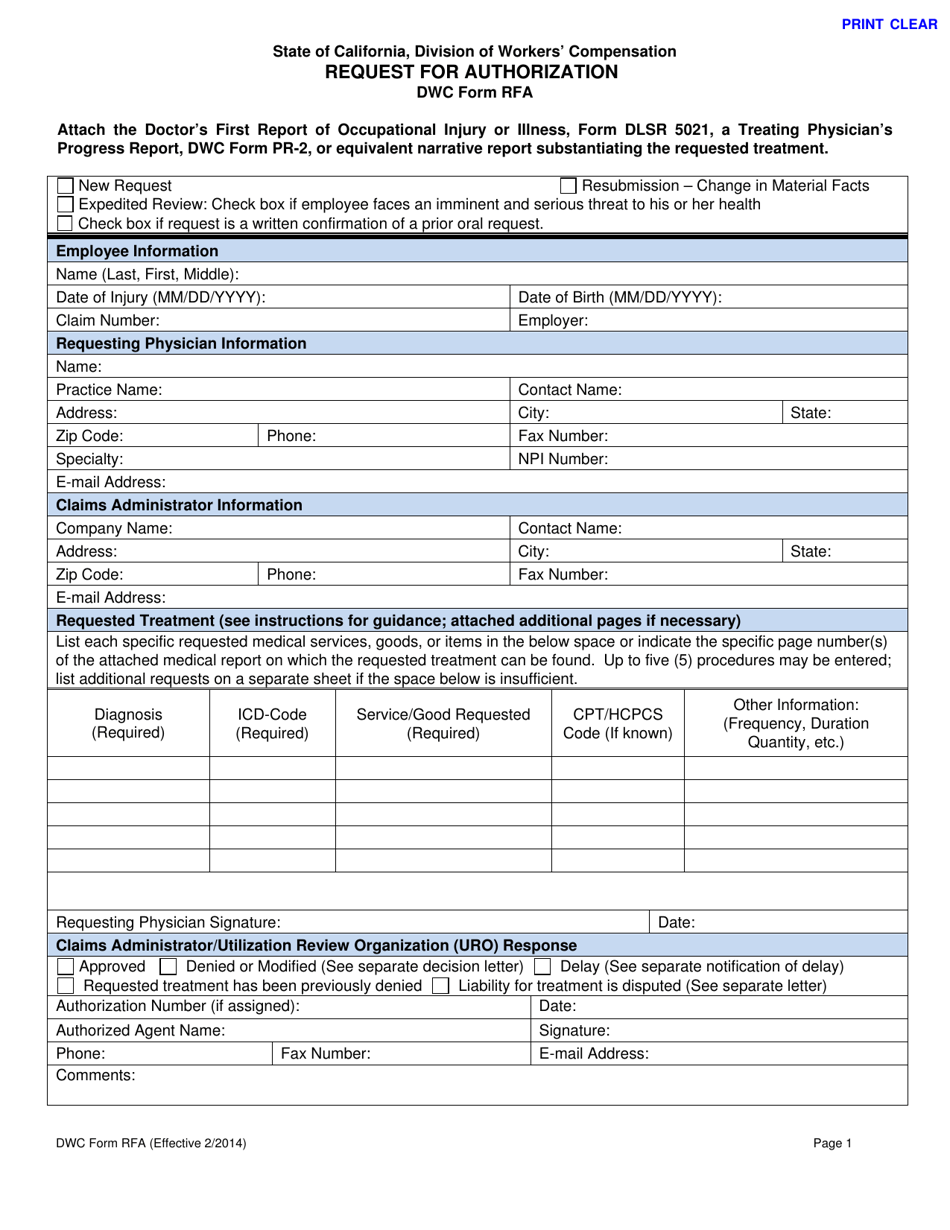
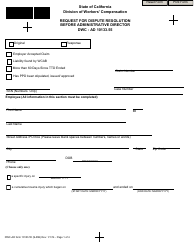
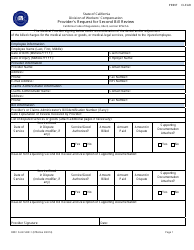
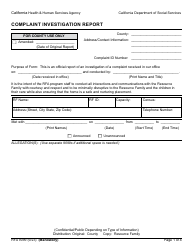
DWC Form RFA, Request for Authorization , is a legal document filled out by the treating physician of the employee with a work-related injury or illness to request authorization of special medical treatment, services, and procedures.
Alternate Names:
- RFA Form;
- DWC Request for Authorization.
The RFA Form must be given to the claims administrator or authorized agent of the utilization review organization in charge of the utilization review process. The claims administrator then reviews the request and determines if this treatment to an industrial injury or illness is medically necessary and appropriate. It is necessary to obtain preauthorization of non-emergency services by identifying recommended treatments and attaching documentation that substantiates the need for the treatment.
This form was released by the California Division of Worker's Compensation , a component of the California Department of Industrial Relations . The latest version of the form was issued on February 1, 2014 , with all previous editions obsolete. You can download a fillable California RFA Form through the link below.
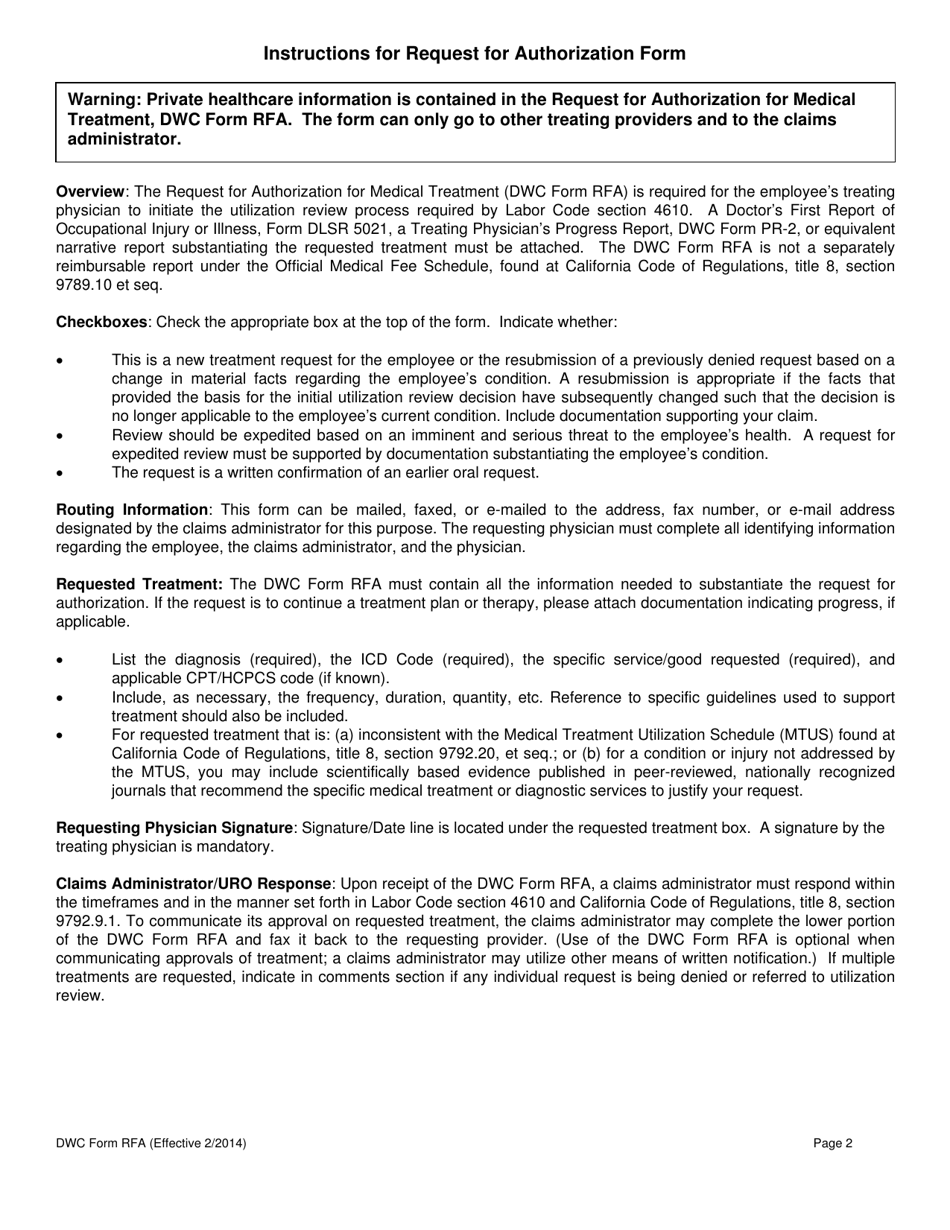
DWC Form RFA Instructions
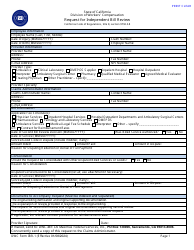
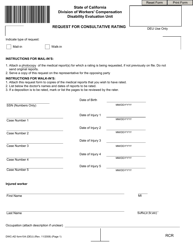
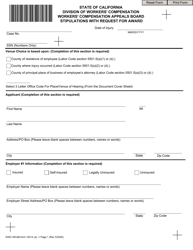
The employee's treating physician needs to provide the following details in the DWC Request for Authorization:
- Specify the type of request. It may be new, expedited (if the employee faces a serious and imminent threat to their health), resubmitted, or written confirmation of a prior oral request;
- Add employee information - full name, date of birth, date of injury, number of the claim, and name of the employer;
- Identify yourself - full name, practice name, contact name, address, phone number, and e-mail address. Specify your specialty and National Provider Identifier number;
- Enter the claims administrator details - the name of the company, contact name, address, phone number, and e-mail address;
- List requested medical goods, items, and services. Name the employee's diagnosis, indicate the International Statistical Classification code of the injury or illness, the American Medical Association's Current Procedural Terminology/Healthcare Common Procedure Coding System code, and provide other information about the treatment (duration, frequency, quantity, etc.). Additional requests must be submitted on a separate sheet if you do not have enough space for it in the request;
- Sign and date the form.
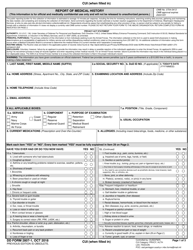
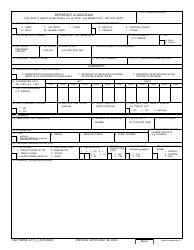
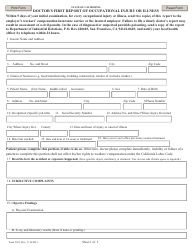
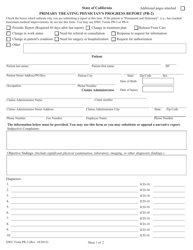
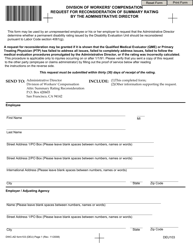
Once the request is filled out, mail, fax, or e-mail it to the address, fax number, or e-mail address is given to you by the claims administrator. You need to attach Form 5021, Doctor's First Report of Occupational Injury or Illness, and DWC Form PR-2, Treating Physician's Progress Report. Then the administrator will approve, modify, deny, or delay the request, notify you the requested treatment has already been denied, or inform you that the liability for the treatment is disputed within five business days of receipt of the request. The authorized agent will write down their authorization number, name, and contact information, date and sign the form.