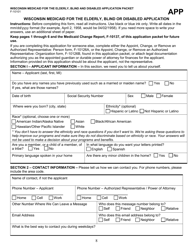
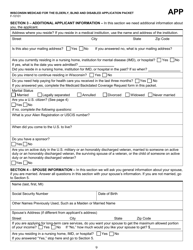
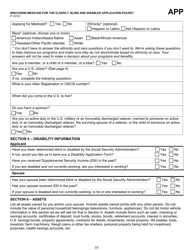
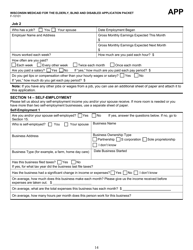
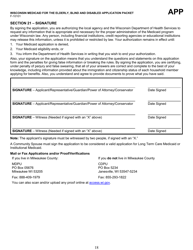
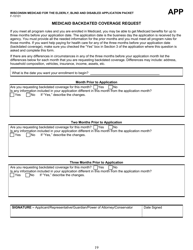
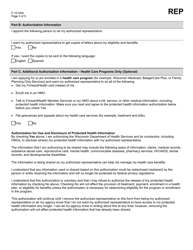
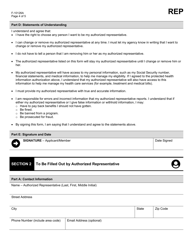
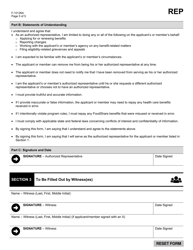
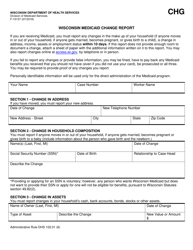
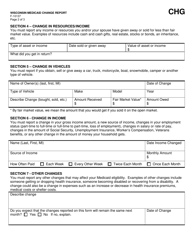
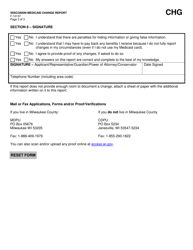
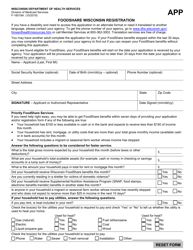
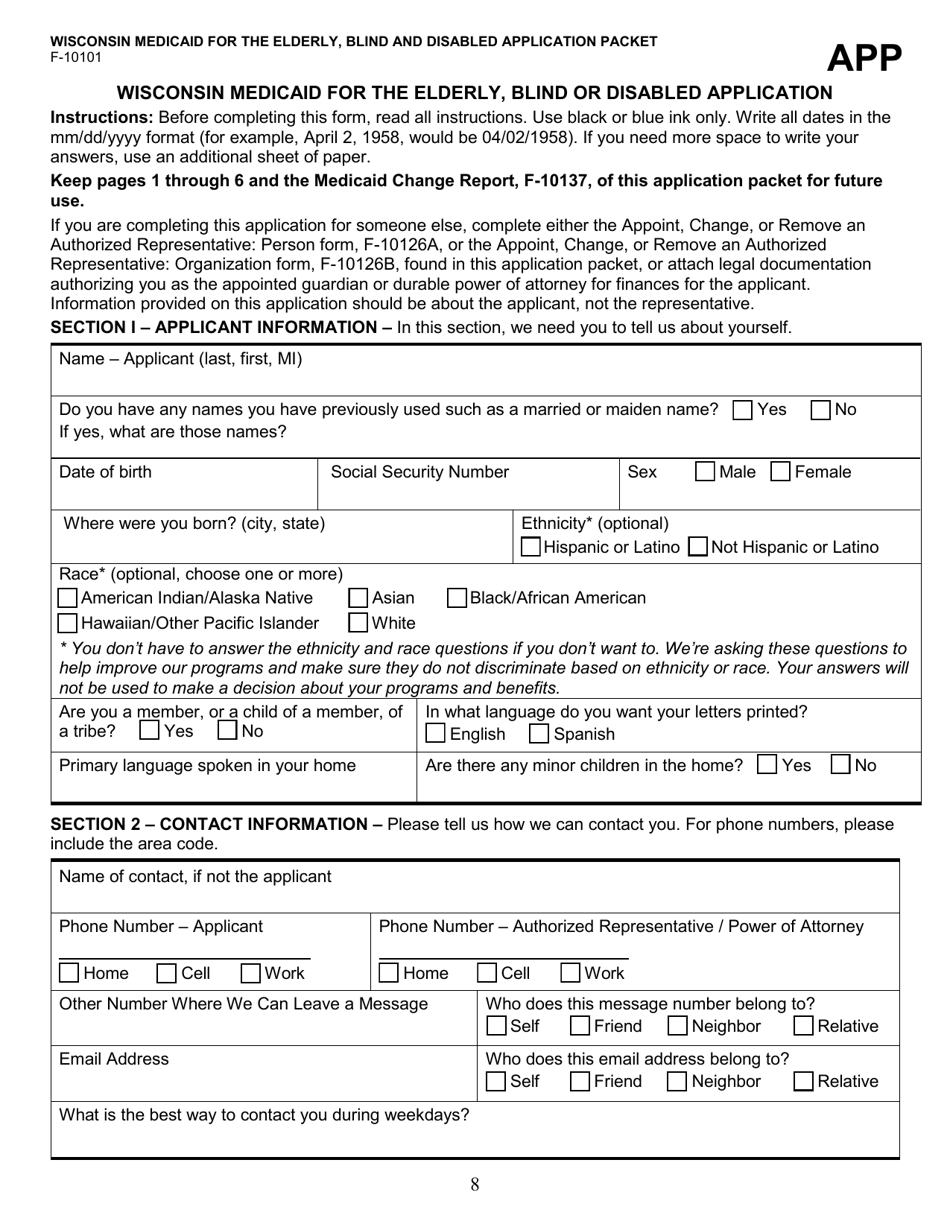
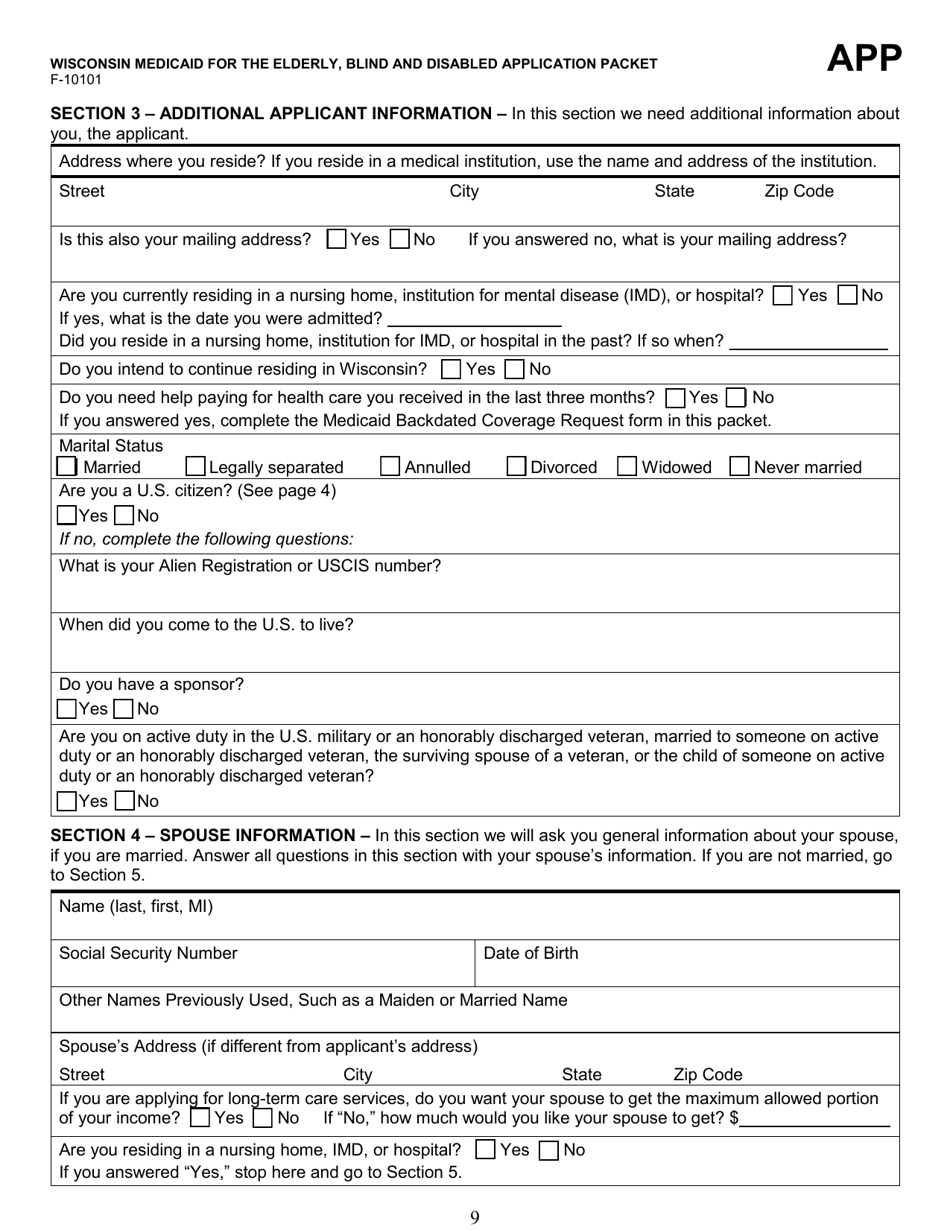
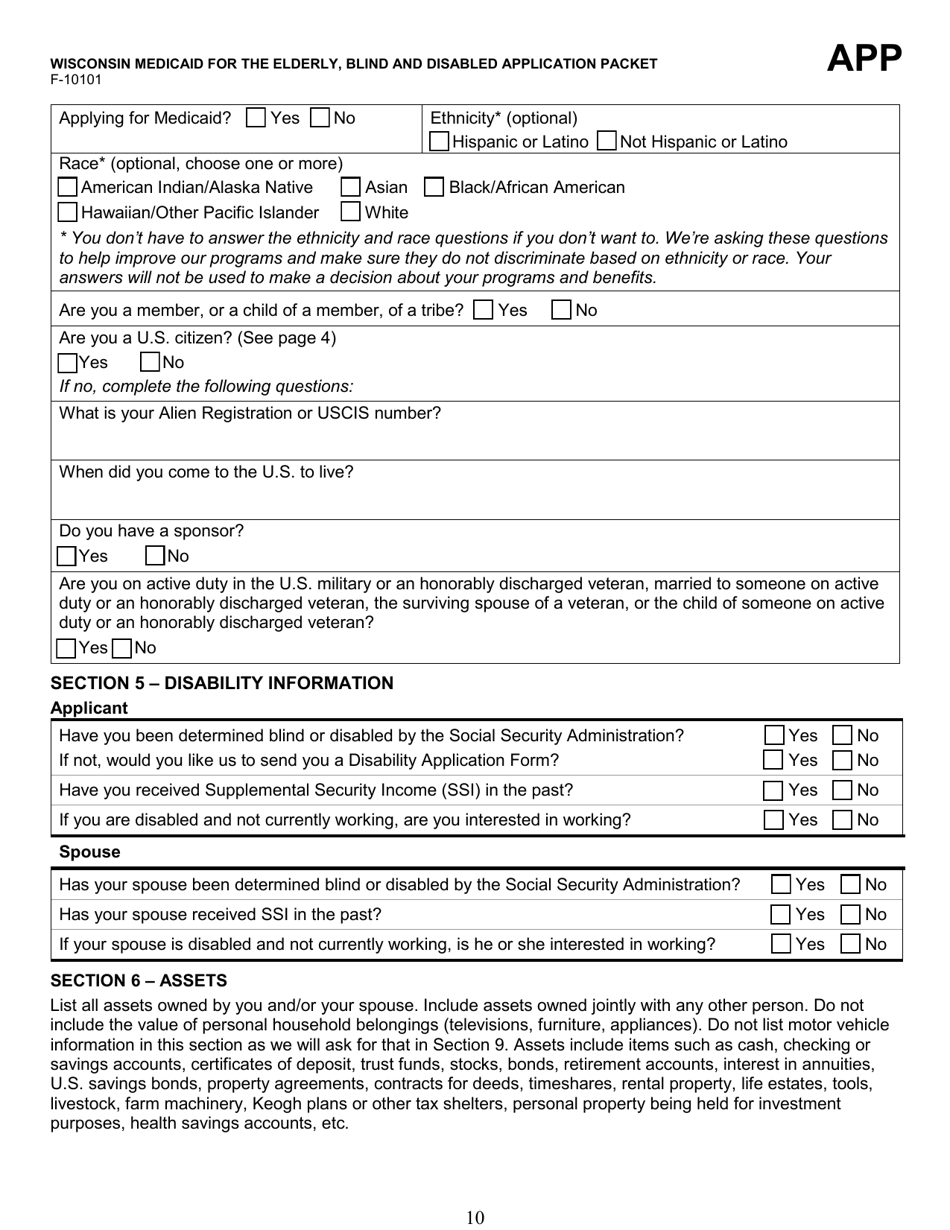
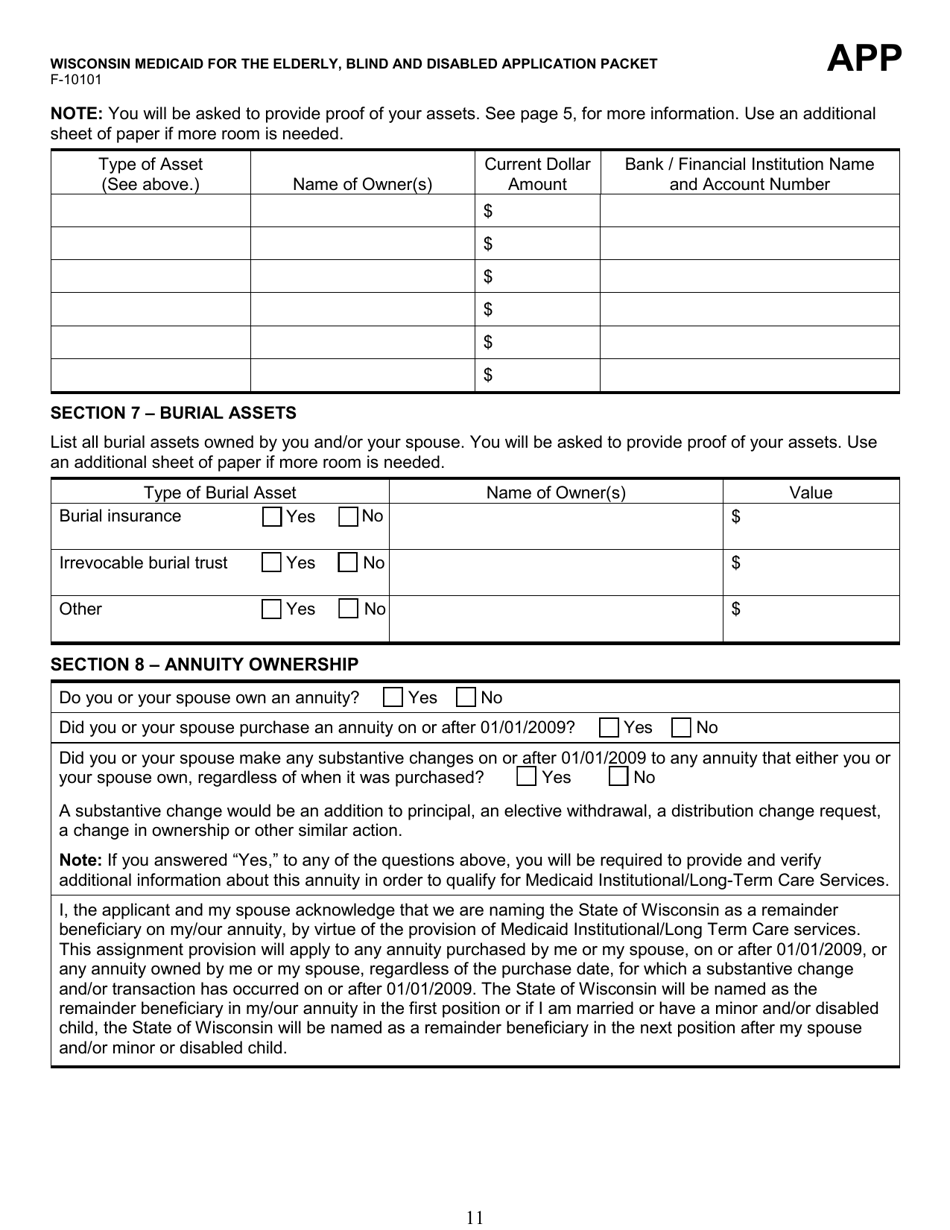
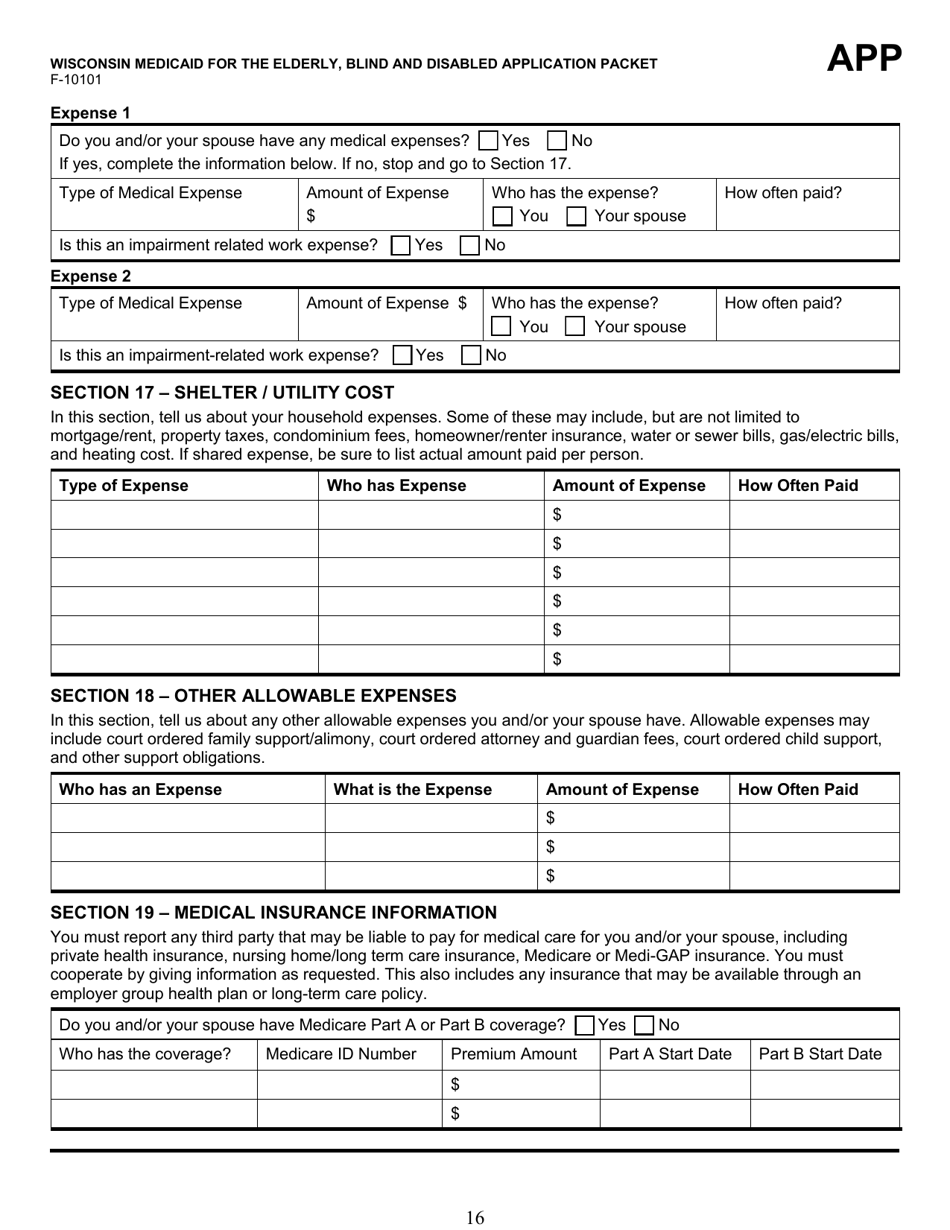
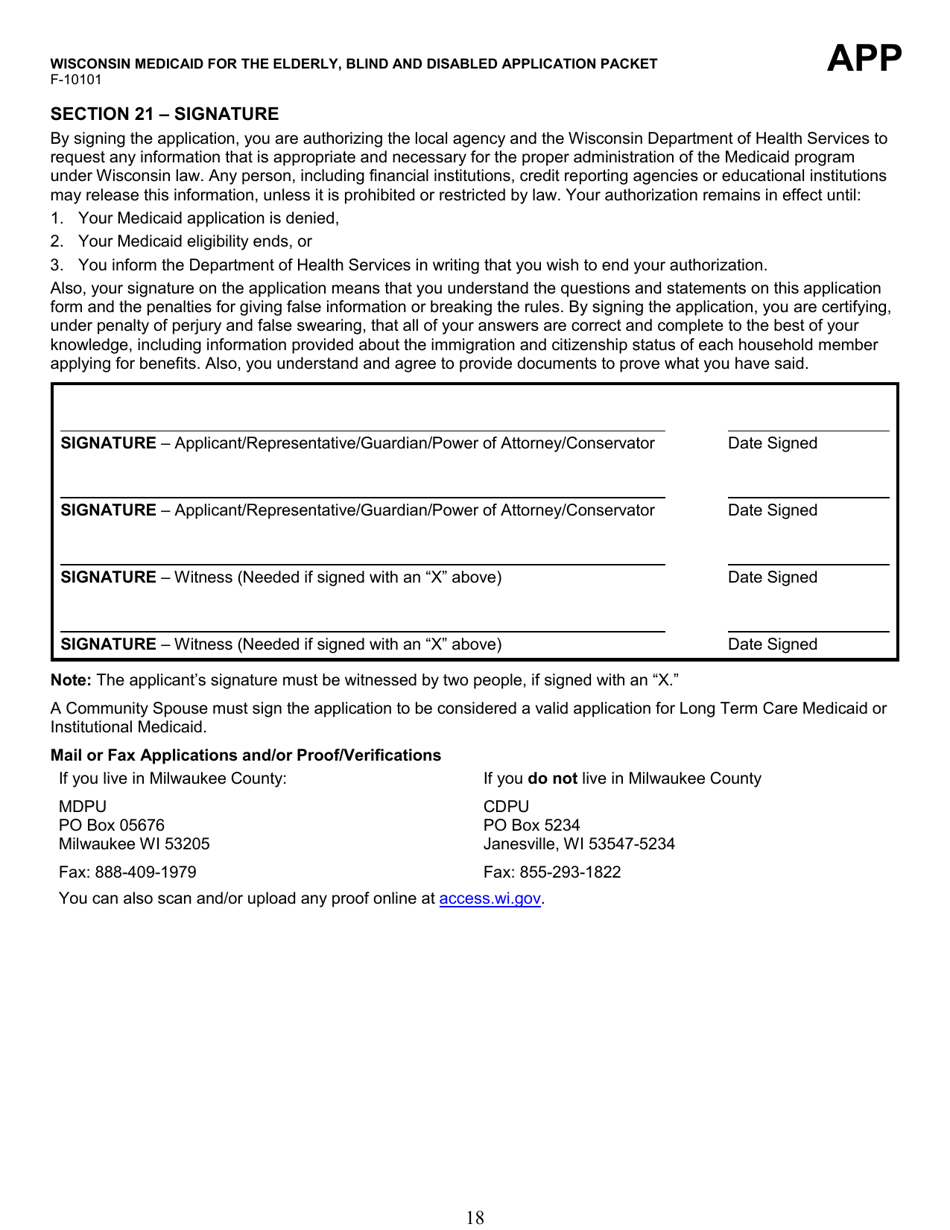
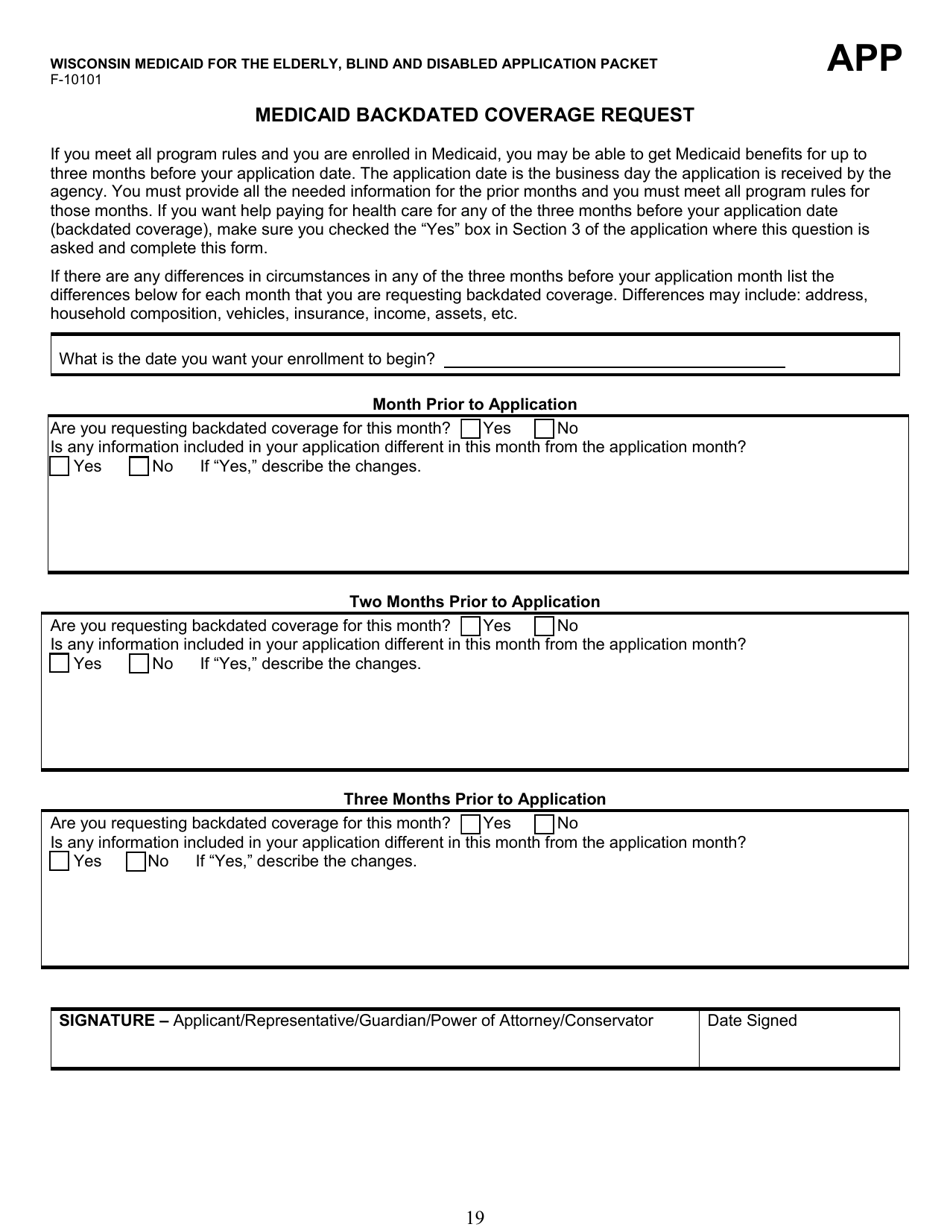
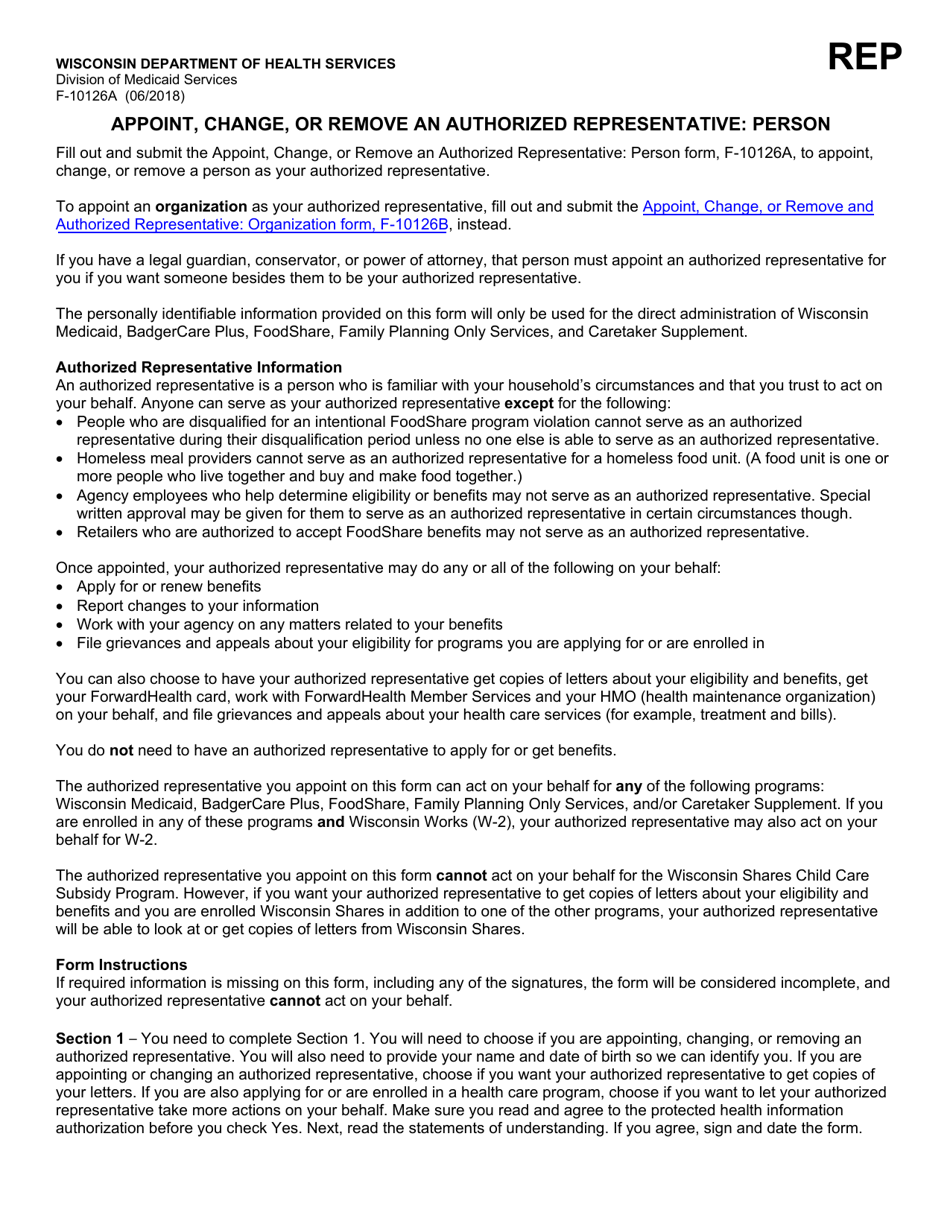
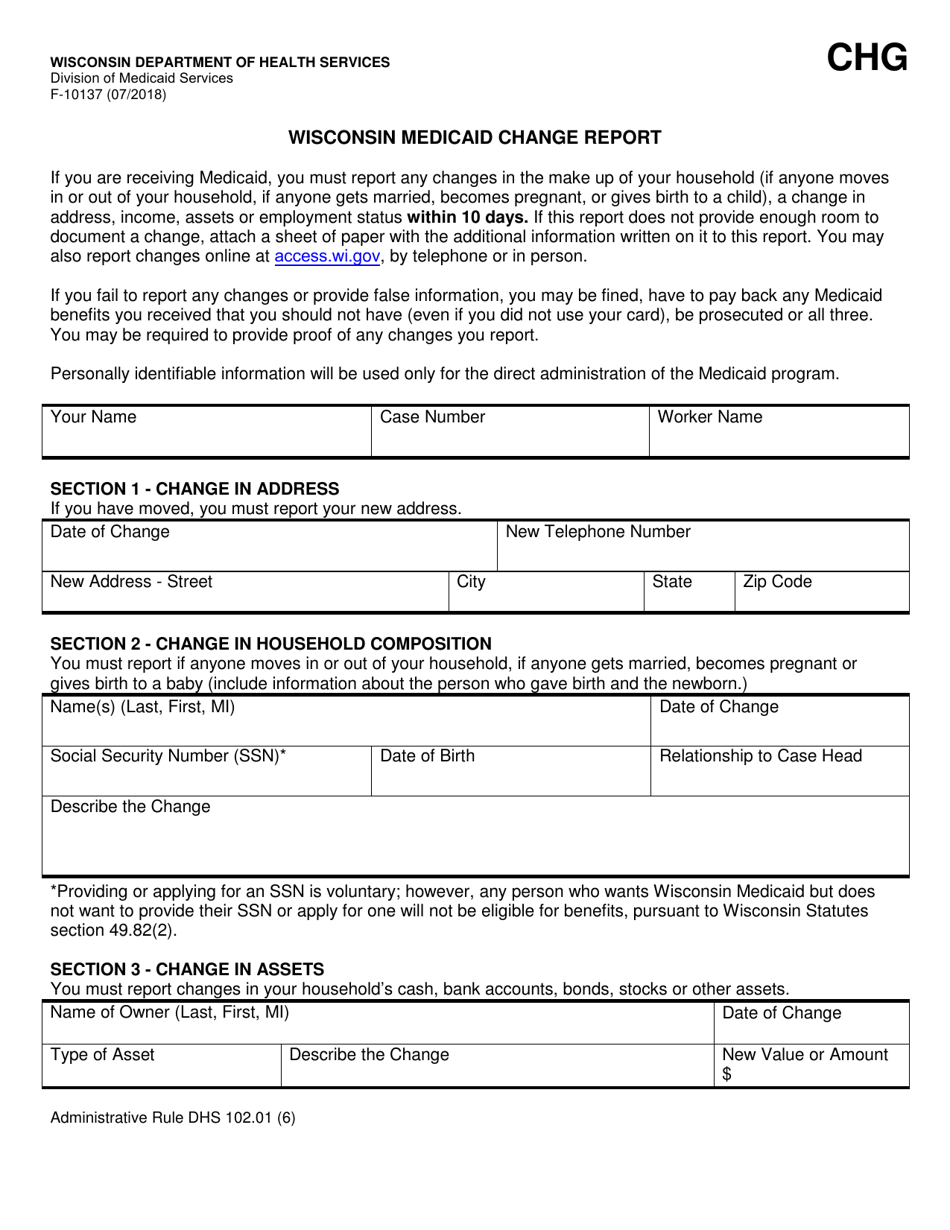
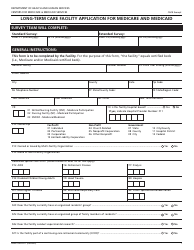
Form F-10101 Wisconsin Medicaid for the Elderly, Blind or Disabled Application Packet - Wisconsin
What Is Form F-10101?
This is a legal form that was released by the Wisconsin Department of Health Services - a government authority operating within Wisconsin. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form F-10101?
A: Form F-10101 is the Wisconsin Medicaid for the Elderly, Blind or Disabled Application Packet.
Q: Who is eligible for Wisconsin Medicaid for the Elderly, Blind or Disabled?
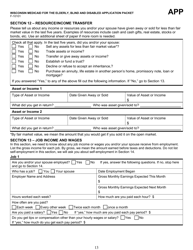
A: Eligibility is based on age, blindness, disability, and income and asset limits.
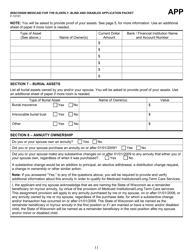
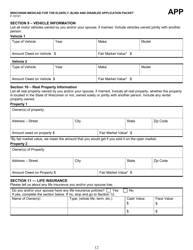
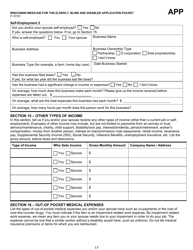
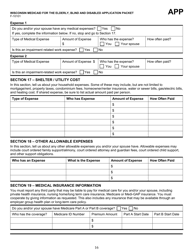
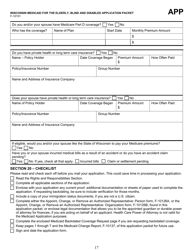
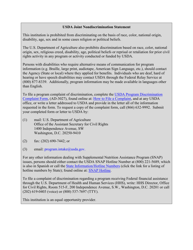
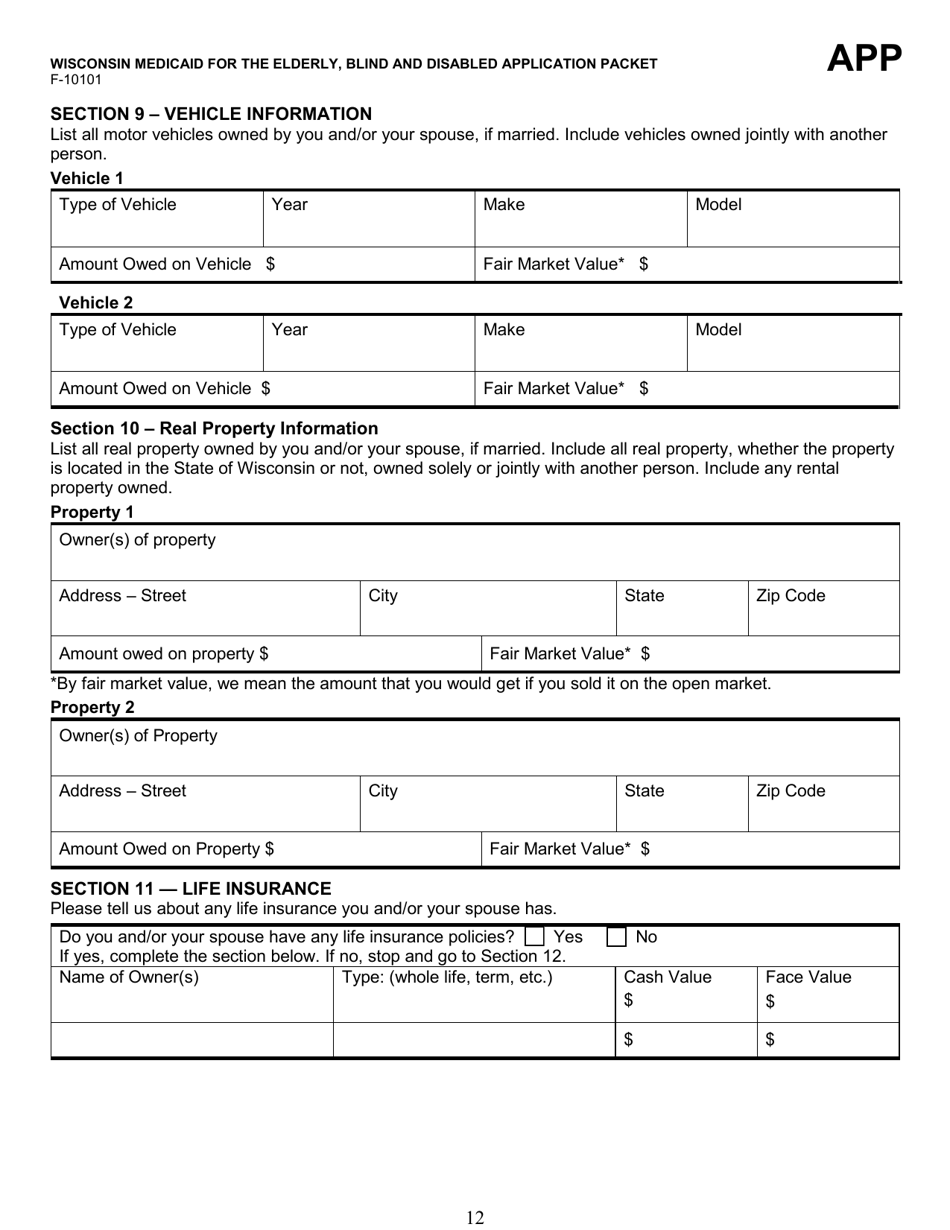
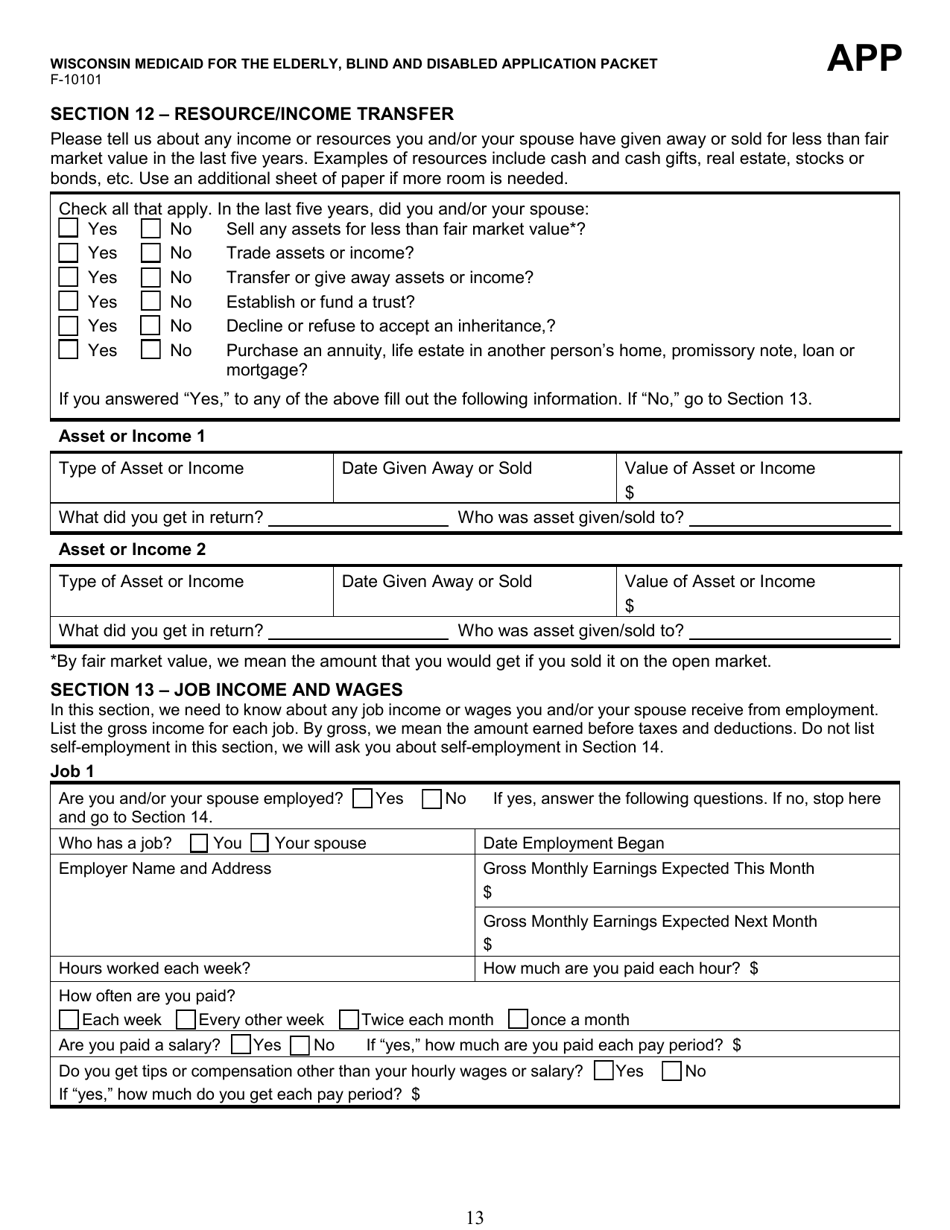
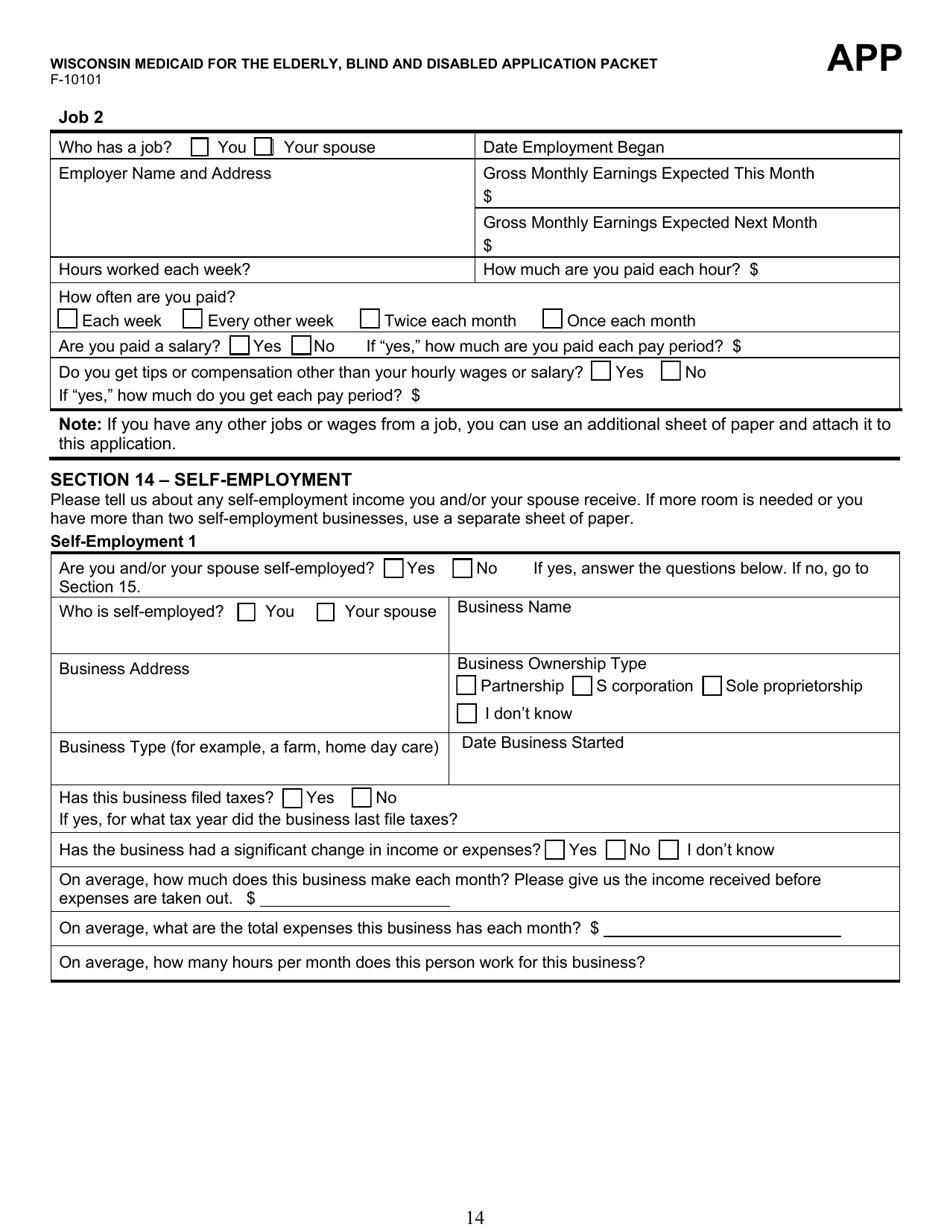
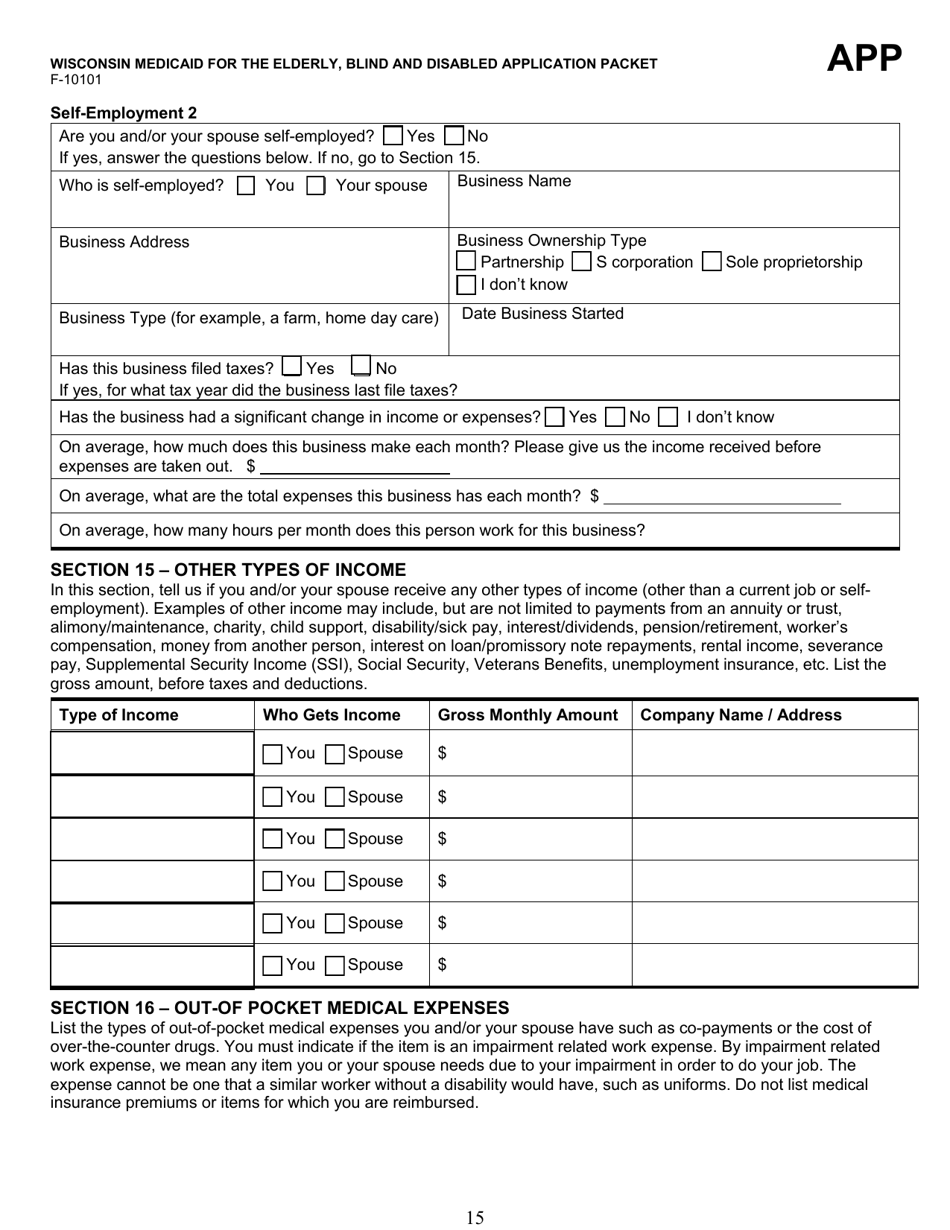
Q: What documents are required for the application?
A: You will need to provide proof of identity, citizenship, income, assets, and medical expenses.
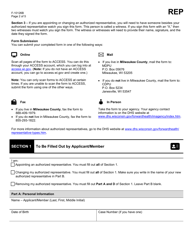
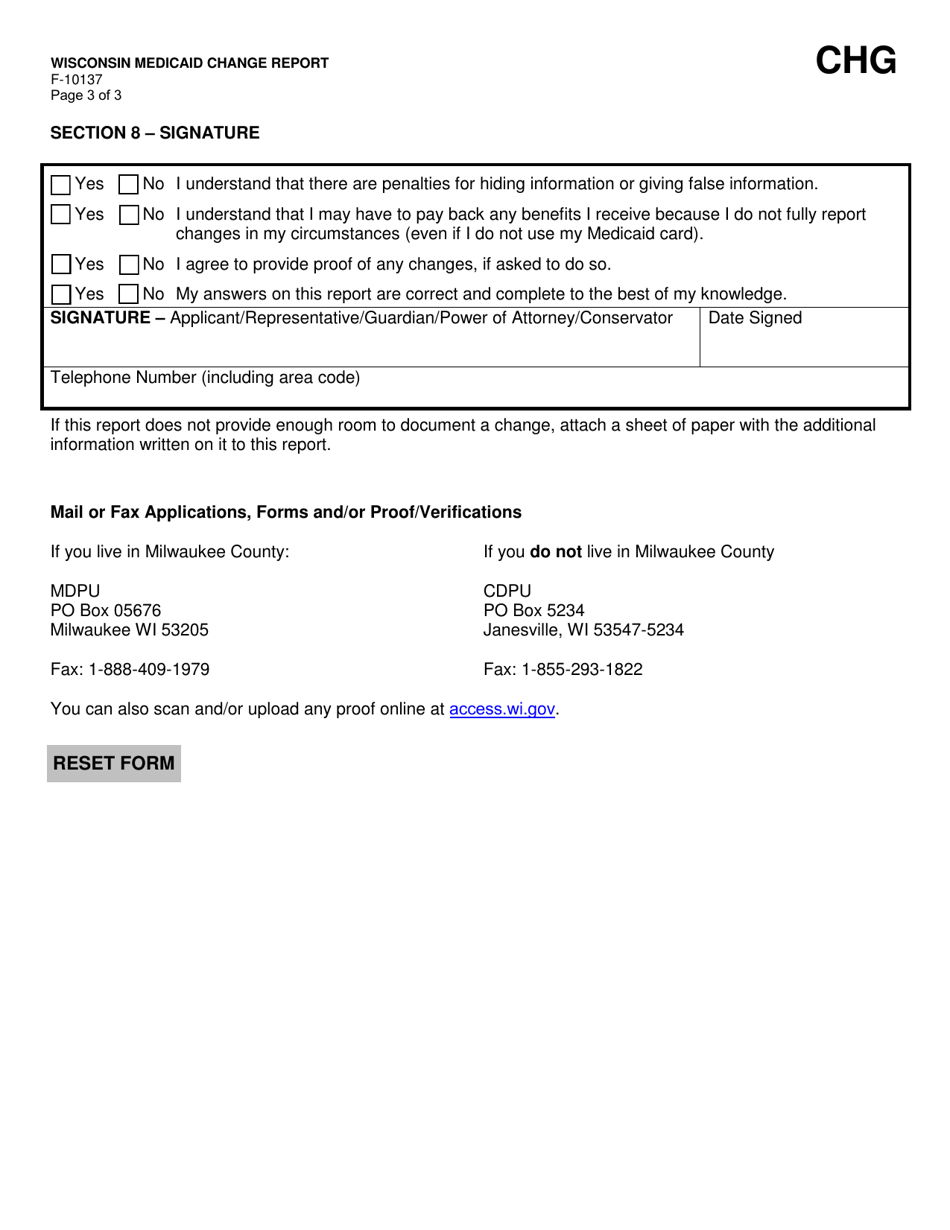
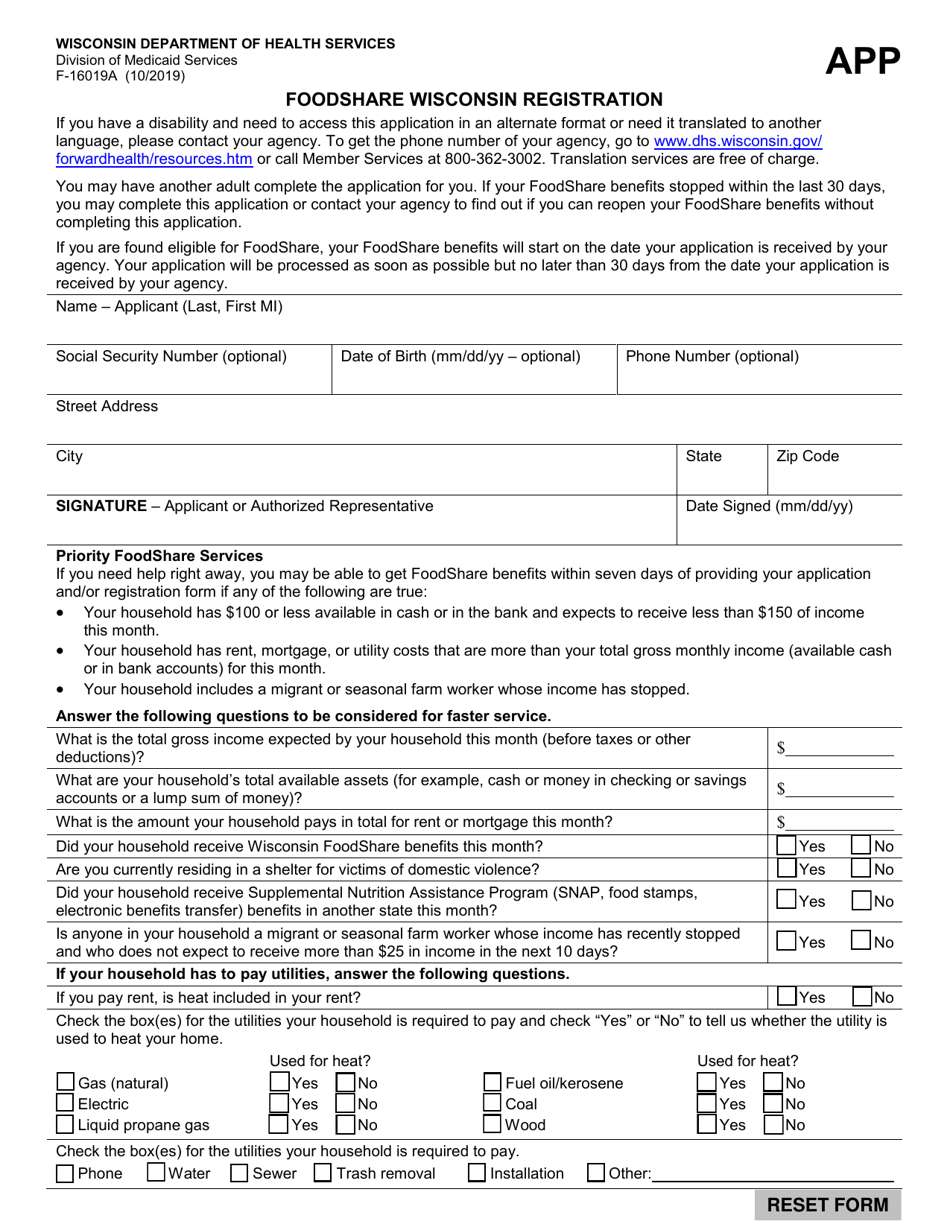
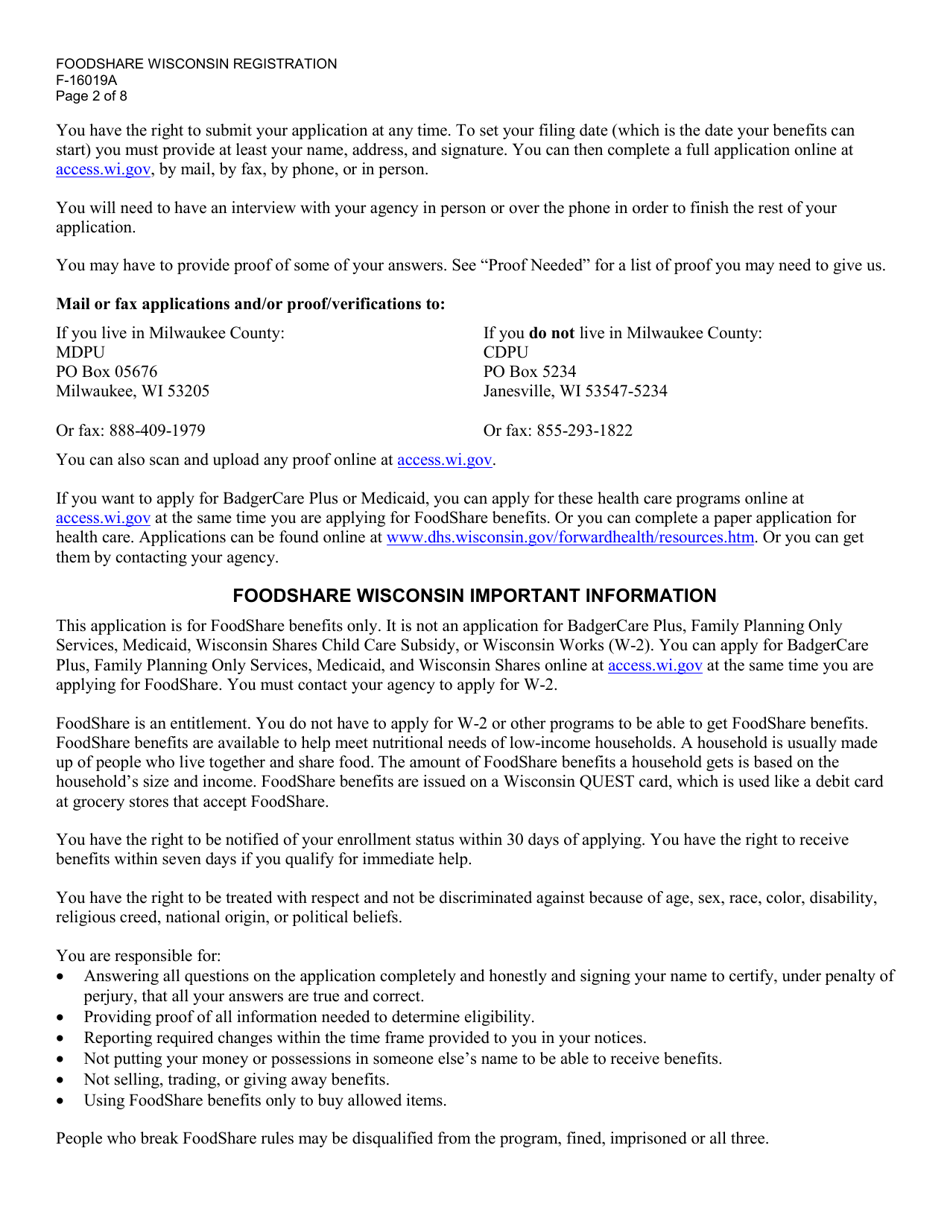
Q: How can I submit my application?
A: You can submit your application by mail, fax, or in person at your local Wisconsin Medicaid office.
Q: How long does it take to process the application?
A: Processing times may vary, but it typically takes about 45 days to process a Wisconsin Medicaid application.
Q: What happens after my application is approved?
A: If your application is approved, you will receive a Wisconsin Medicaid card and be enrolled in the program.
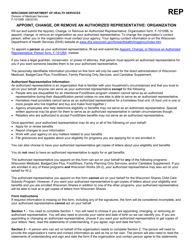
Q: What if I need assistance with the application process?
A: If you need assistance with the application process, you can contact your local Wisconsin Medicaid office or seek help from a Medicaid enrollment specialist.
Form Details:
- Released on February 1, 2020;
- The latest edition provided by the Wisconsin Department of Health Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form F-10101 by clicking the link below or browse more documents and templates provided by the Wisconsin Department of Health Services.