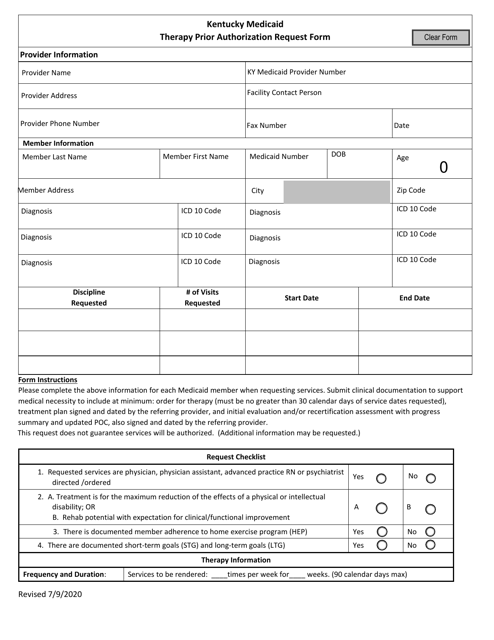
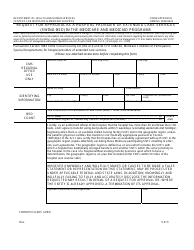
Kentucky Medicaid Therapy Prior Authorization Request Form - Kentucky
Kentucky Medicaid Therapy Prior Authorization Request Form is a legal document that was released by the Kentucky Department for Medicaid Services - a government authority operating within Kentucky.
FAQ
Q: What is the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: The Kentucky Medicaid Therapy Prior Authorization Request Form is a document used to request prior authorization for therapy services under Kentucky Medicaid.
Q: Why is prior authorization needed for therapy services under Medicaid?
A: Prior authorization is needed to ensure that therapy services are medically necessary and meet the eligibility criteria set by Medicaid.
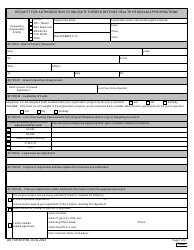
Q: Who needs to complete the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: The form needs to be completed by the healthcare provider or therapist requesting prior authorization for therapy services.
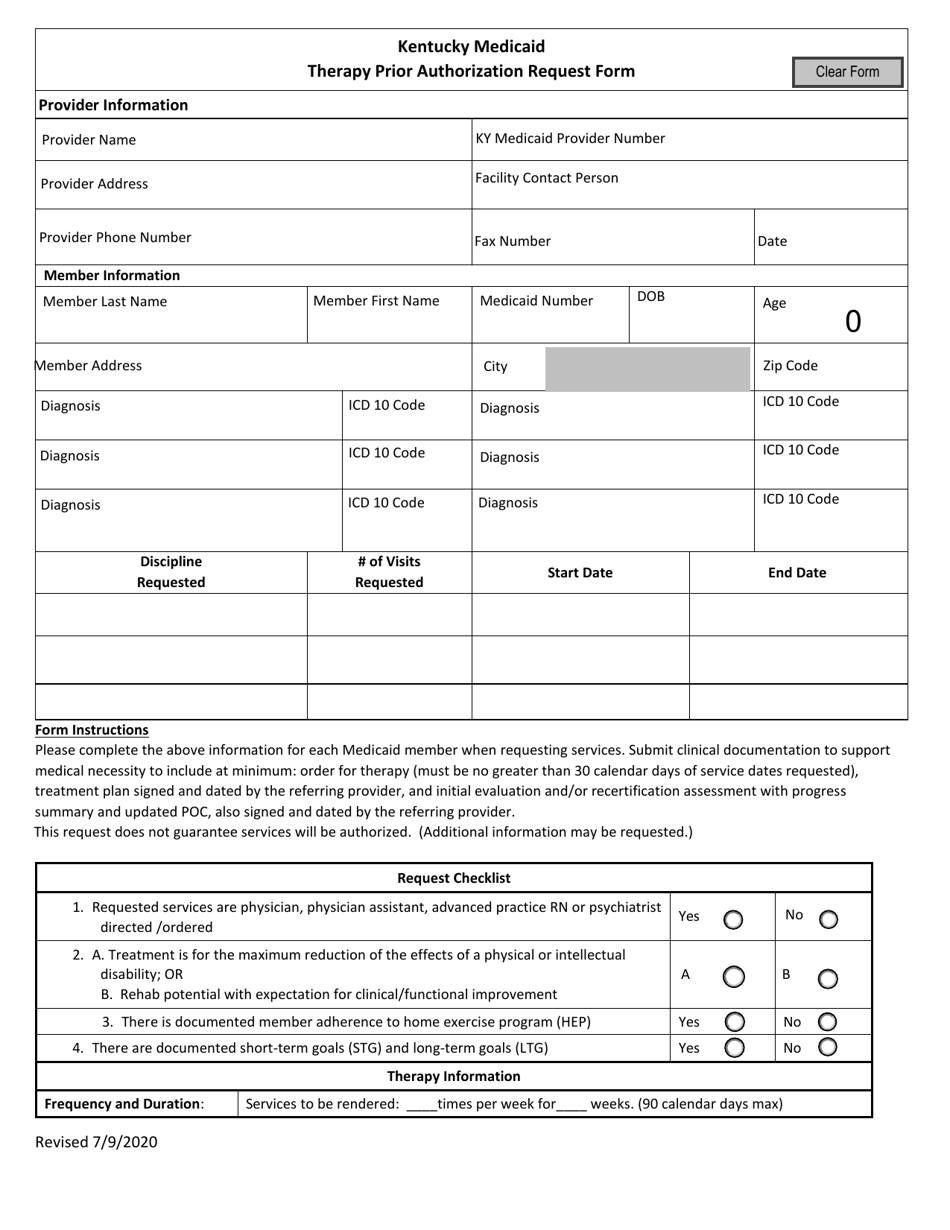
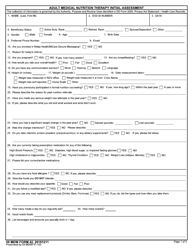
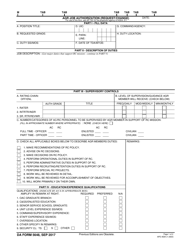
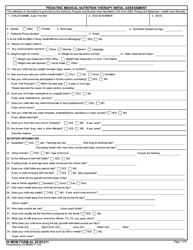
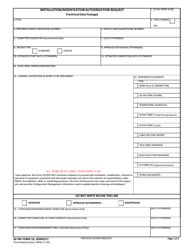
Q: What information is required on the Kentucky Medicaid Therapy Prior Authorization Request Form?
A: The form requires the patient's demographic information, diagnosis, type of therapy requested, and supporting documentation.
Q: How long does it take to get a response for a prior authorization request?
A: The timeframe for a response to a prior authorization request may vary, but typically it takes a few days to a few weeks depending on the urgency of the situation.
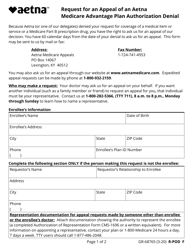
Q: What should I do if my prior authorization request is denied?
A: If your prior authorization request is denied, you can appeal the decision and provide additional documentation or justification for the therapy services.
Q: Can I start therapy services before receiving prior authorization?
A: Starting therapy services before receiving prior authorization may result in the services not being covered by Medicaid, so it is recommended to wait for approval before starting.
Q: Are there any exceptions to the prior authorization requirement for therapy services?
A: Some therapy services may be exempt from the prior authorization requirement, such as emergency or urgent care situations. It is best to check with the Kentucky Medicaid program for specific guidelines.
Q: Is there a specific timeframe for how long therapy services are authorized for?
A: The timeframe for authorized therapy services may vary depending on the individual's needs and the recommendation of the healthcare provider. It can range from a few weeks to several months.
Form Details:
- Released on July 9, 2020;
- The latest edition currently provided by the Kentucky Department for Medicaid Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the Kentucky Department for Medicaid Services.