This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
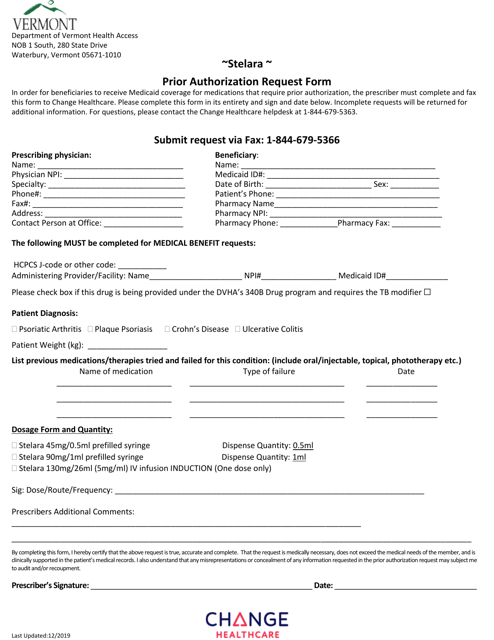
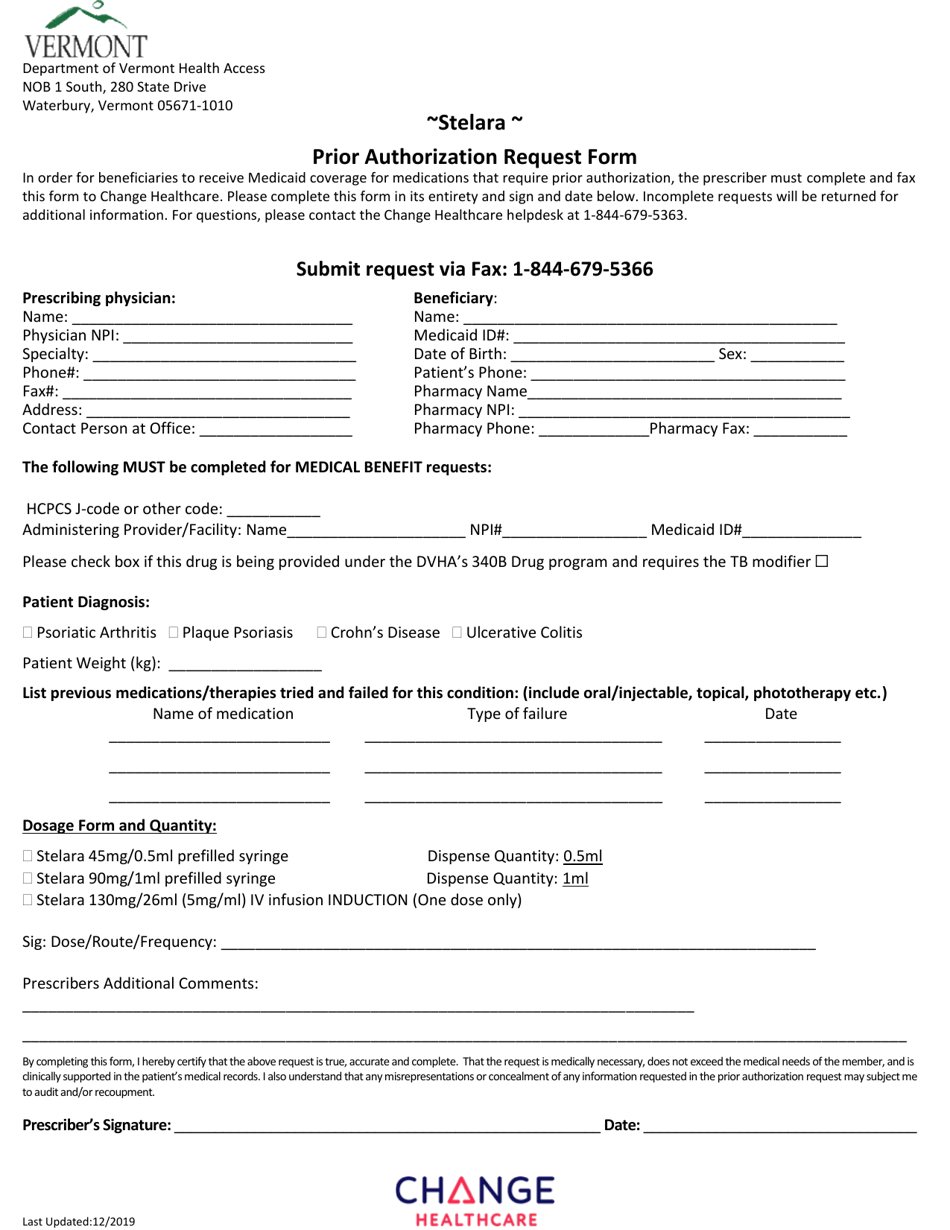
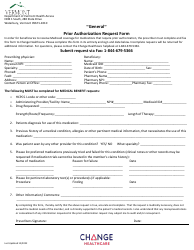
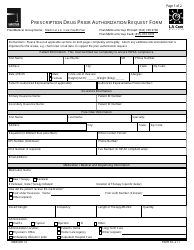
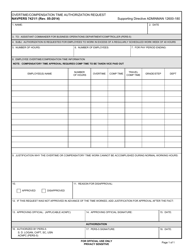
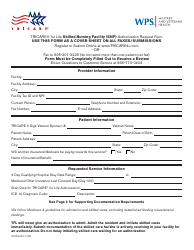
Stelara Prior Authorization Request Form - Vermont
Stelara Prior Authorization Request Form is a legal document that was released by the Department of Vermont Health Access - a government authority operating within Vermont.
FAQ
Q: What is a Stelara Prior Authorization Request Form?
A: A Stelara Prior Authorization Request Form is a document used in Vermont to request approval from the insurance company for the medication Stelara.
Q: What is Stelara?
A: Stelara is a medication used to treat certain immune-mediated conditions, such as psoriasis and psoriatic arthritis.
Q: Why do I need a prior authorization for Stelara?
A: Insurance companies often require a prior authorization before covering the cost of certain medications, including Stelara. This helps ensure that the medication is medically necessary and appropriate for the patient.
Q: How do I obtain a Stelara Prior Authorization Request Form?
A: You can obtain a Stelara Prior Authorization Request Form from your healthcare provider or by contacting your insurance company directly.
Q: What information is needed on the Stelara Prior Authorization Request Form?
A: The form typically requires information such as the patient's diagnosis, medical history, prescribing healthcare provider's information, and supporting documentation.
Q: What happens after I submit the Stelara Prior Authorization Request Form?
A: After you submit the form, the insurance company will review the request and determine whether or not to approve coverage for Stelara. They may also require additional information or documentation.
Q: How long does it take to get a decision on a Stelara Prior Authorization Request?
A: The timeframe for a decision on a prior authorization request can vary depending on the insurance company. It is best to check with your insurance provider for an estimated timeline.
Q: What if my Stelara Prior Authorization Request is denied?
A: If your request is denied, you can often file an appeal with your insurance company. Your healthcare provider can help you with the appeals process.
Q: Is there a cost associated with the Stelara Prior Authorization Request Form?
A: The Stelara Prior Authorization Request Form itself does not typically have a cost. However, the medication itself may have a cost, depending on your insurance coverage.
Form Details:
- Released on December 1, 2019;
- The latest edition currently provided by the Department of Vermont Health Access;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Department of Vermont Health Access.