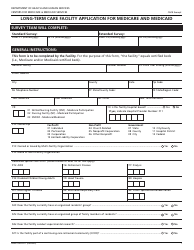
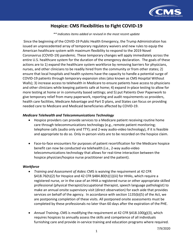
Long Term Care Facilities (Skilled Nursing Facilities and / or Nursing Facilities): Cms Flexibilities to Fight Covid-19
Long Term Nursing Facilities and/or Nursing Facilities): Cms Flexibilities to Fight Covid-19 is a 11-page legal document that was released by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services on July 9, 2020 and used nation-wide.
FAQ
Q: What are long term care facilities?
A: Long term care facilities are places that provide skilled nursing and/or nursing care.
Q: What is CMS?
A: CMS stands for the Centers for Medicare & Medicaid Services, which is a federal agency that oversees healthcare programs such as Medicare and Medicaid.
Q: What is Covid-19?
A: Covid-19 is a respiratory illness caused by the coronavirus.
Q: What flexibilities has CMS provided to long term care facilities during Covid-19?
A: CMS has provided flexibilities to help long term care facilities fight Covid-19, such as allowing temporary nursing aides, relaxing certain staffing requirements, and implementing infection control protocols.
Q: What are temporary nursing aides?
A: Temporary nursing aides are individuals who can be trained and employed to assist with direct patient care during the Covid-19 pandemic.
Q: What staffing requirements have been relaxed?
A: CMS has relaxed certain staffing requirements, such as allowing facilities to use volunteers or individuals not certified as nurse aides to provide care.
Q: What are infection control protocols?
A: Infection control protocols are procedures and practices put in place to prevent the spread of infections, such as Covid-19, within a healthcare facility.
Form Details:
- The latest edition currently provided by the U.S. Department of Health and Human Services - Centers for Medicare and Medicaid Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more legal forms and templates provided by the issuing department.