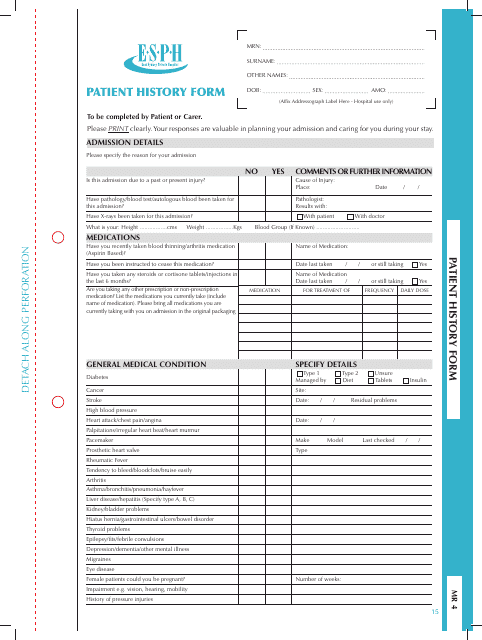
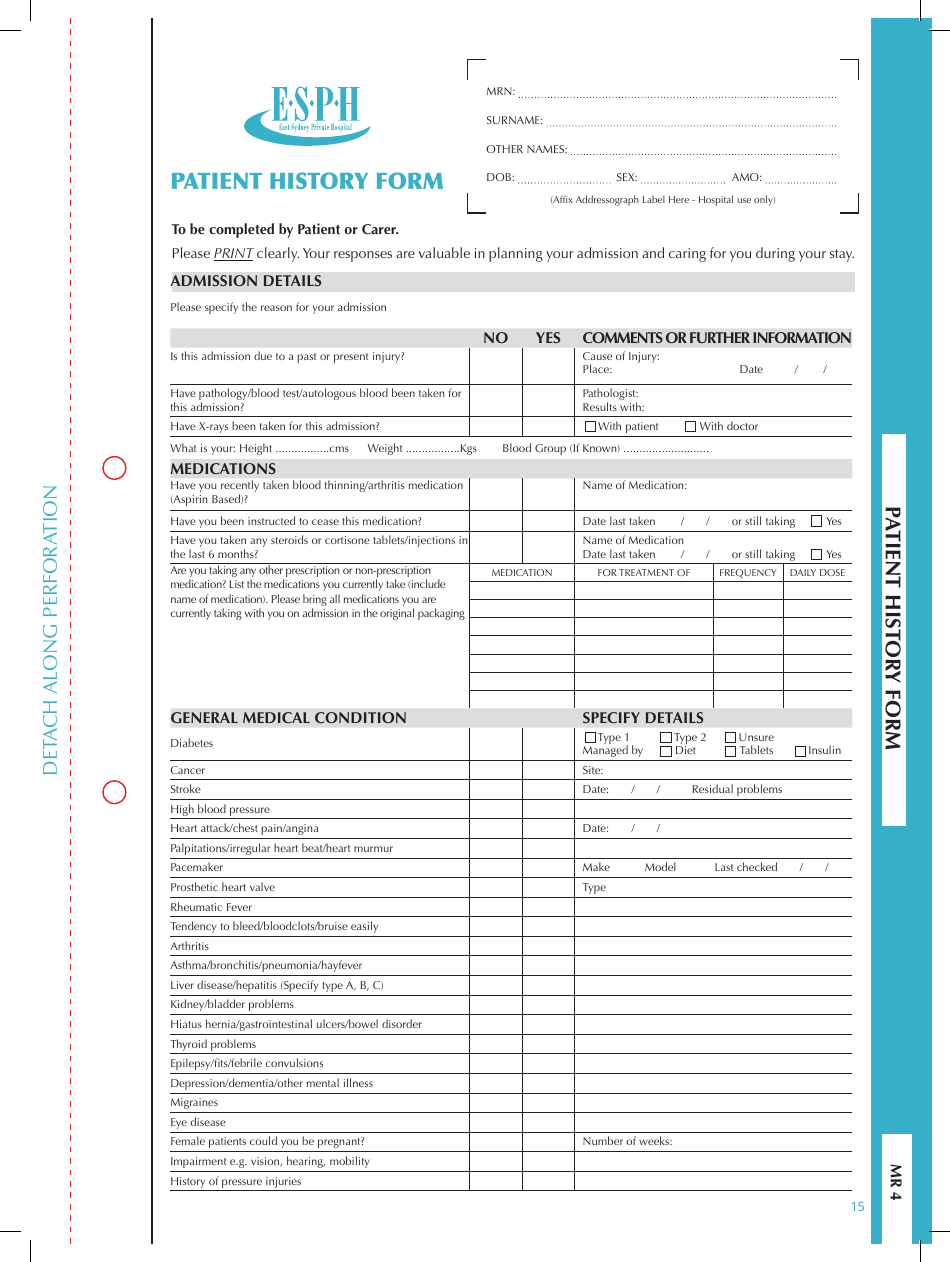
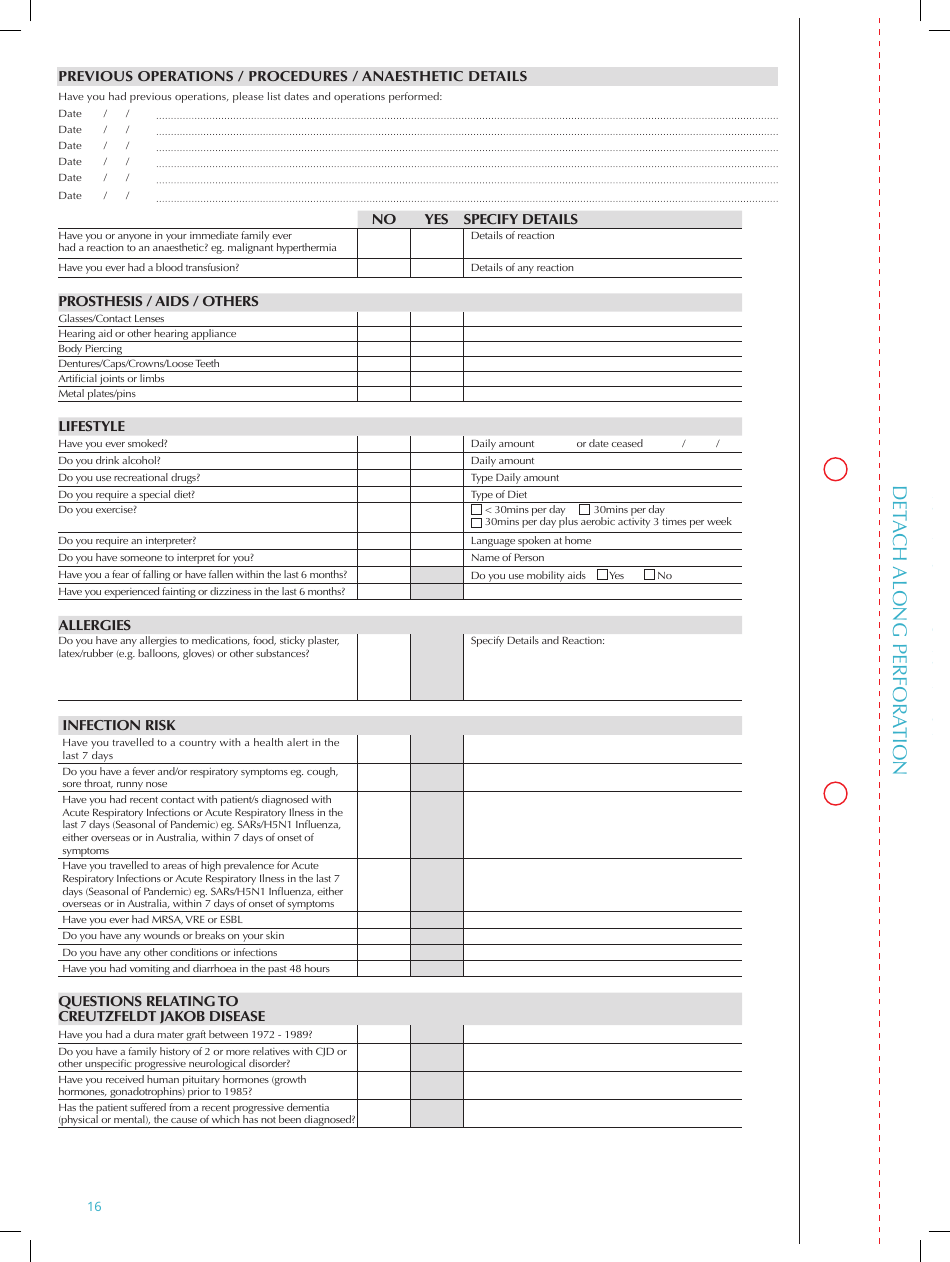
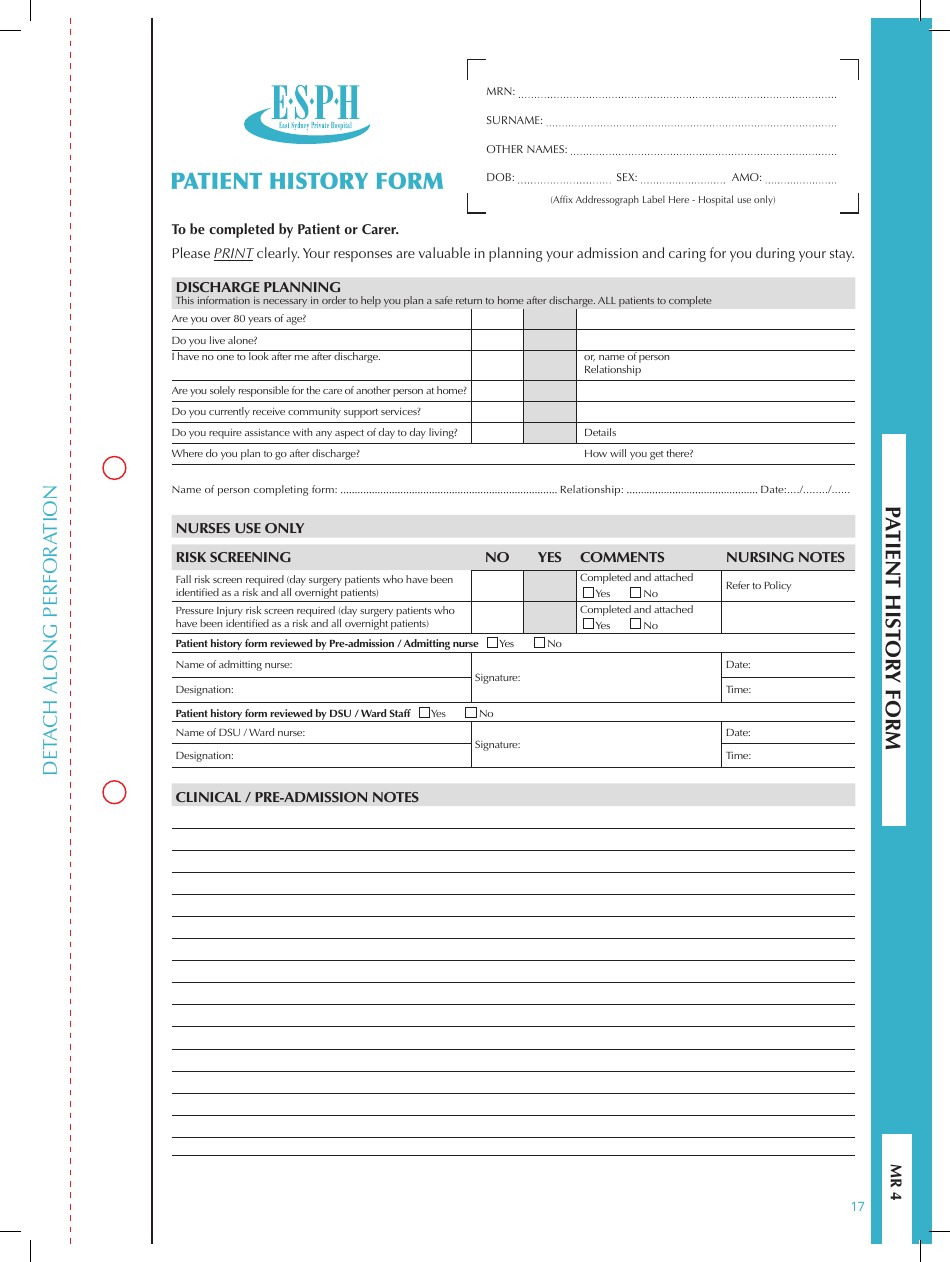
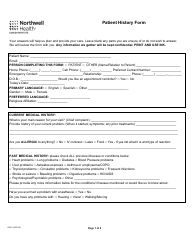
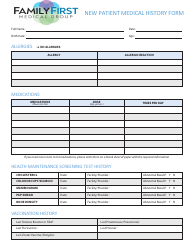
Patient History Form - Esph
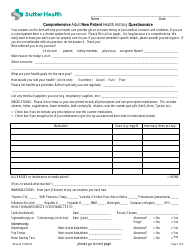
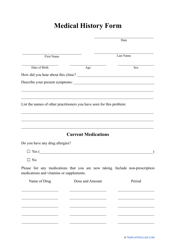
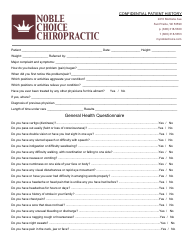
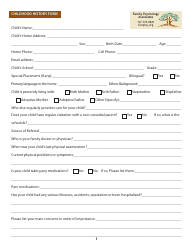
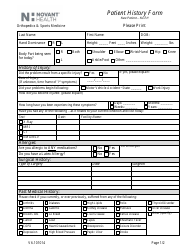
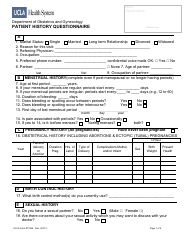
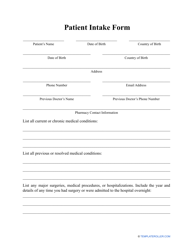
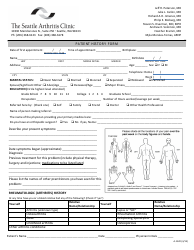
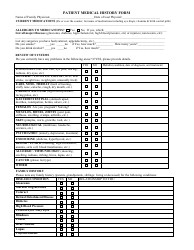
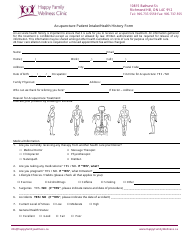
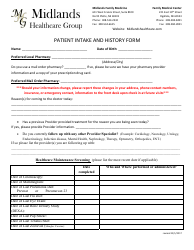
The Patient History Form - Esph is used to collect information about a patient's medical history, current health status, and any previous treatments or conditions. It helps healthcare providers make informed decisions about the patient's care.
FAQ
Q: What is the purpose of a patient history form?
A: The purpose of a patient history form is to gather important medical information about a patient before their appointment or visit.
Q: What information is typically included in a patient history form?
A: A patient history form typically includes personal information, medical history, medications, allergies, and any specific concerns or symptoms the patient may have.
Q: Why is it important to fill out a patient history form accurately?
A: It is important to fill out a patient history form accurately to ensure that healthcare providers have all the necessary information to provide the best possible care for the patient.
Q: Is the information provided on a patient history form confidential?
A: Yes, the information provided on a patient history form is confidential and protected by privacy laws.
Q: Can I update my patient history form if there are any changes in my medical information?
A: Yes, it is important to keep your patient history form up to date to ensure healthcare providers have the most accurate and current information about your health.