Cobra Coverage Templates
Cobra coverage, also known as Cobra continuation services, is an essential resource for individuals who have recently experienced a change in their employment or family status. This collection of documents provides all the necessary information and forms needed to enroll in and maintain Cobra coverage.
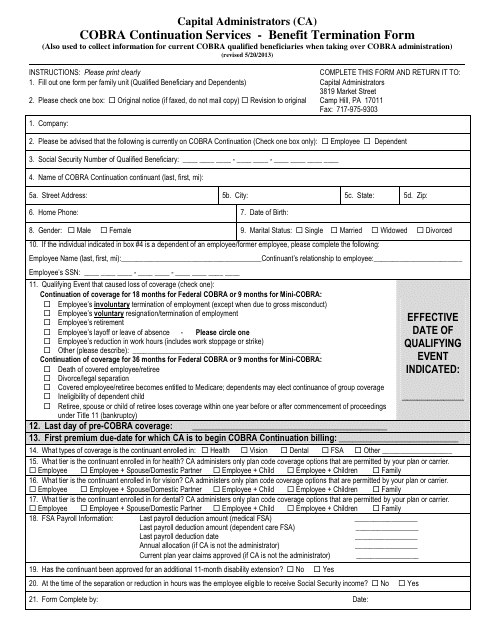
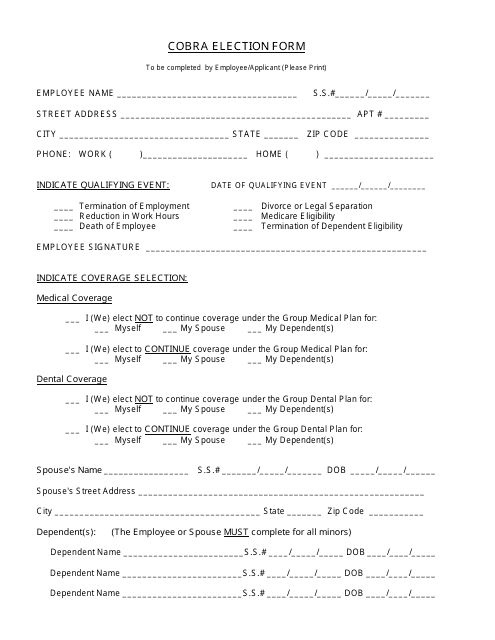
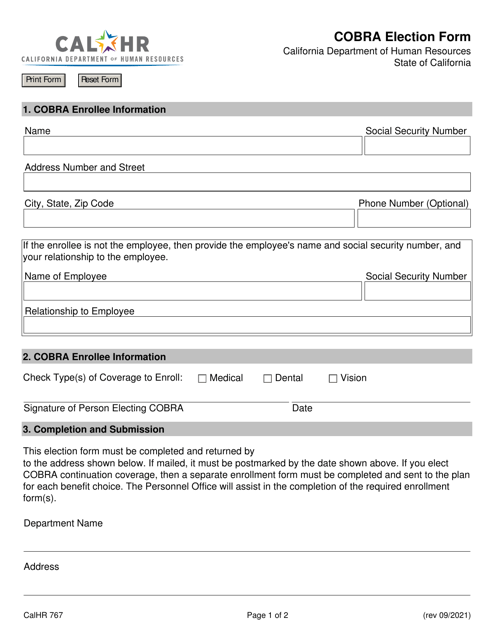
When you find yourself facing a termination of benefits in the state of California, the Benefit Termination Form can guide you through the process. Additionally, for those who are eligible for Cobra coverage, the Cobra Election Form enables you to make an informed decision about continuing your health insurance.
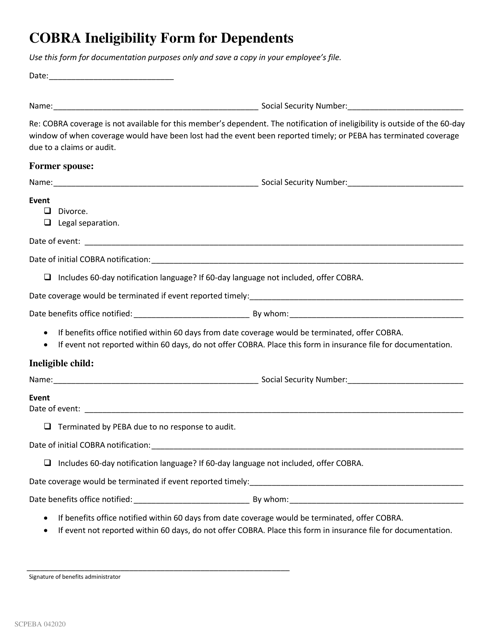
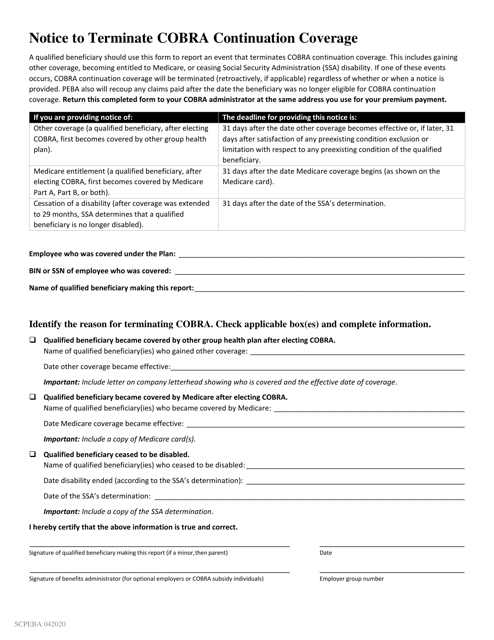
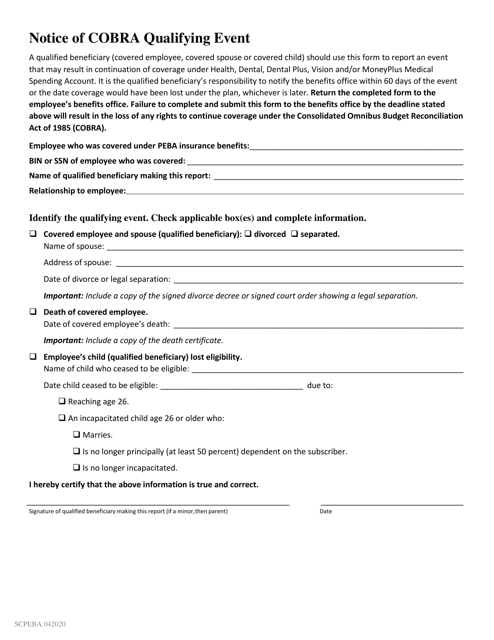
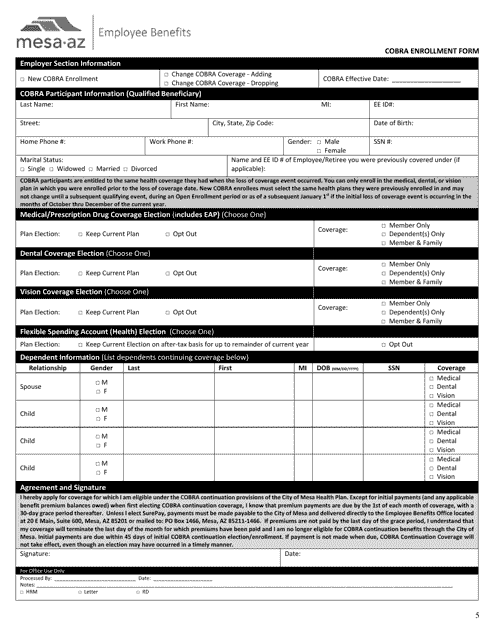
In the state of South Carolina, dependents who are deemed ineligible for Cobra coverage can make use of the Cobra Ineligibility Form, while the City of Mesa, Arizona offers its residents the Cobra Enrollment Form to facilitate the enrollment process.
Whether you're seeking to understand your rights and options under Cobra coverage or need specific forms to fulfill your obligations, this comprehensive collection of documents has you covered. Explore the resources available to you and ensure that you have the necessary information to make the best decisions for your healthcare needs.
Documents:
8
This Form is used for terminating benefits with Cobra Continuation Services in California.
This document provides essential information for employees about their health benefits under COBRA. It covers topics such as eligibility, coverage duration, and the rights and responsibilities of employees.
This form is used for dependents who are ineligible for Cobra coverage in South Carolina.
This document is a notice that is used to terminate COBRA continuation coverage in South Carolina.
This document is a notice regarding a qualifying event for COBRA in South Carolina. COBRA refers to the Consolidated Omnibus Budget Reconciliation Act, which provides temporary continuation of group health coverage in certain situations. The notice informs individuals of a qualifying event that may entitle them to COBRA coverage.
This Form is used for enrolling in the Cobra healthcare program offered by the City of Mesa, Arizona.