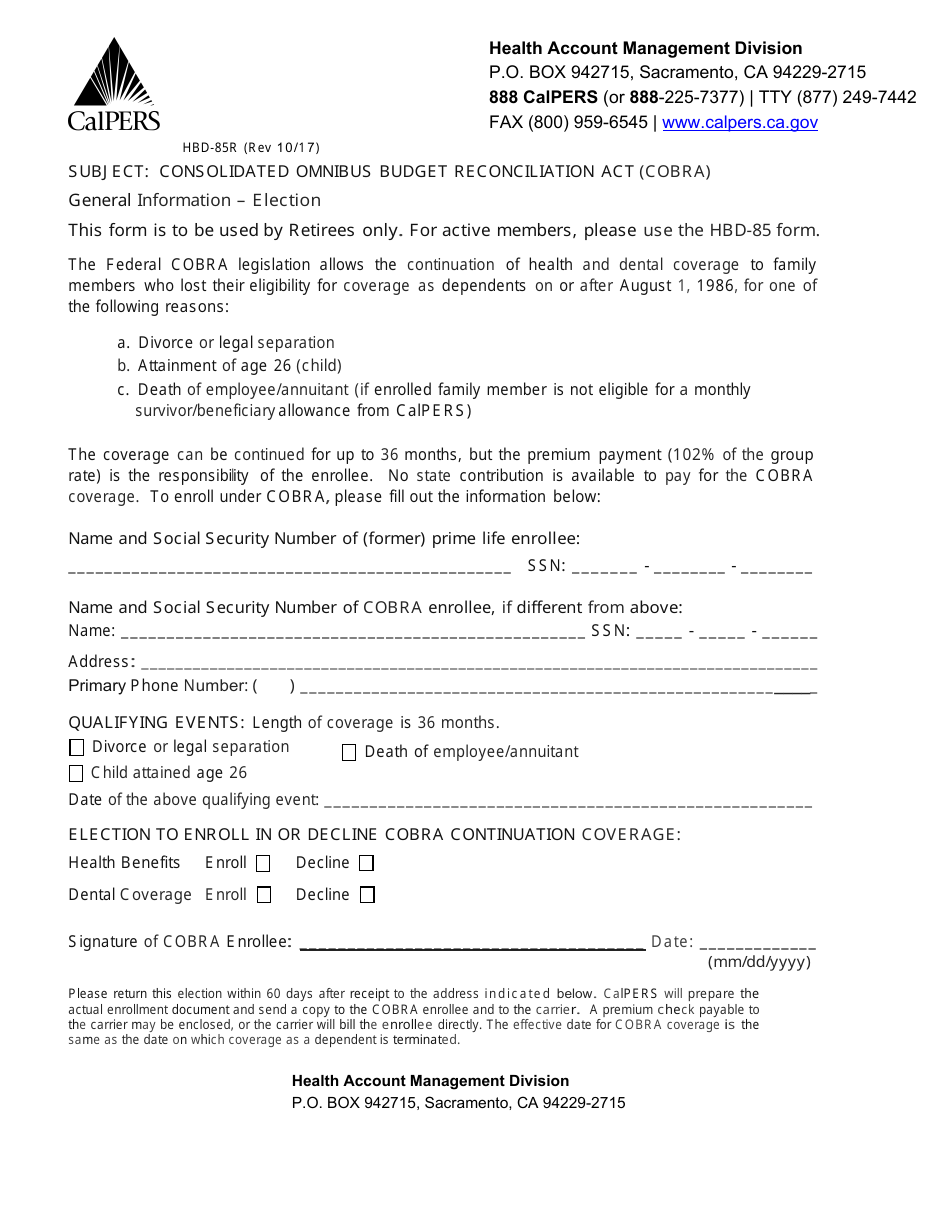
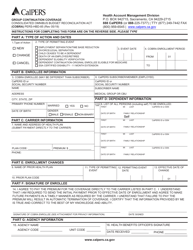
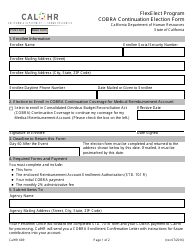
Form HBD-85R Cobra Election Form (Retirees) - California
What Is Form HBD-85R?
This is a legal form that was released by the California Public Employees' Retirement System - a government authority operating within California. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
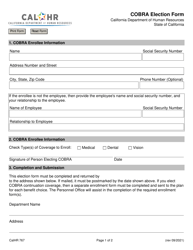
Q: What is Form HBD-85R?
A: Form HBD-85R is the Cobra election form for retirees in California.
Q: Who is eligible to use Form HBD-85R?
A: Retirees in California who are eligible for Cobra coverage can use Form HBD-85R.
Q: What is Cobra coverage?
A: Cobra coverage is a continuation of health insurance coverage for qualified individuals after their employment ends.
Q: Why do retirees need to fill out Form HBD-85R?
A: Retirees need to fill out Form HBD-85R to elect or decline Cobra coverage.
Q: Are there any deadlines for submitting Form HBD-85R?
A: Yes, retirees must submit Form HBD-85R within 60 days of their coverage termination date to elect Cobra coverage.
Q: Can retirees change their election after submitting Form HBD-85R?
A: No, retirees cannot change their election after submitting Form HBD-85R.
Q: What happens if retirees do not elect Cobra coverage using Form HBD-85R?
A: If retirees do not elect Cobra coverage using Form HBD-85R, they may lose their health insurance benefits.
Q: Is there a cost associated with Cobra coverage?
A: Yes, there is a cost associated with Cobra coverage. Retirees are responsible for paying the full premium.
Q: Can retirees include their dependents in Cobra coverage?
A: Yes, retirees can include their dependents in Cobra coverage, but there may be additional costs.
Form Details:
- Released on October 1, 2017;
- The latest edition provided by the California Public Employees' Retirement System;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form HBD-85R by clicking the link below or browse more documents and templates provided by the California Public Employees' Retirement System.