This version of the form is not currently in use and is provided for reference only. Download this version of
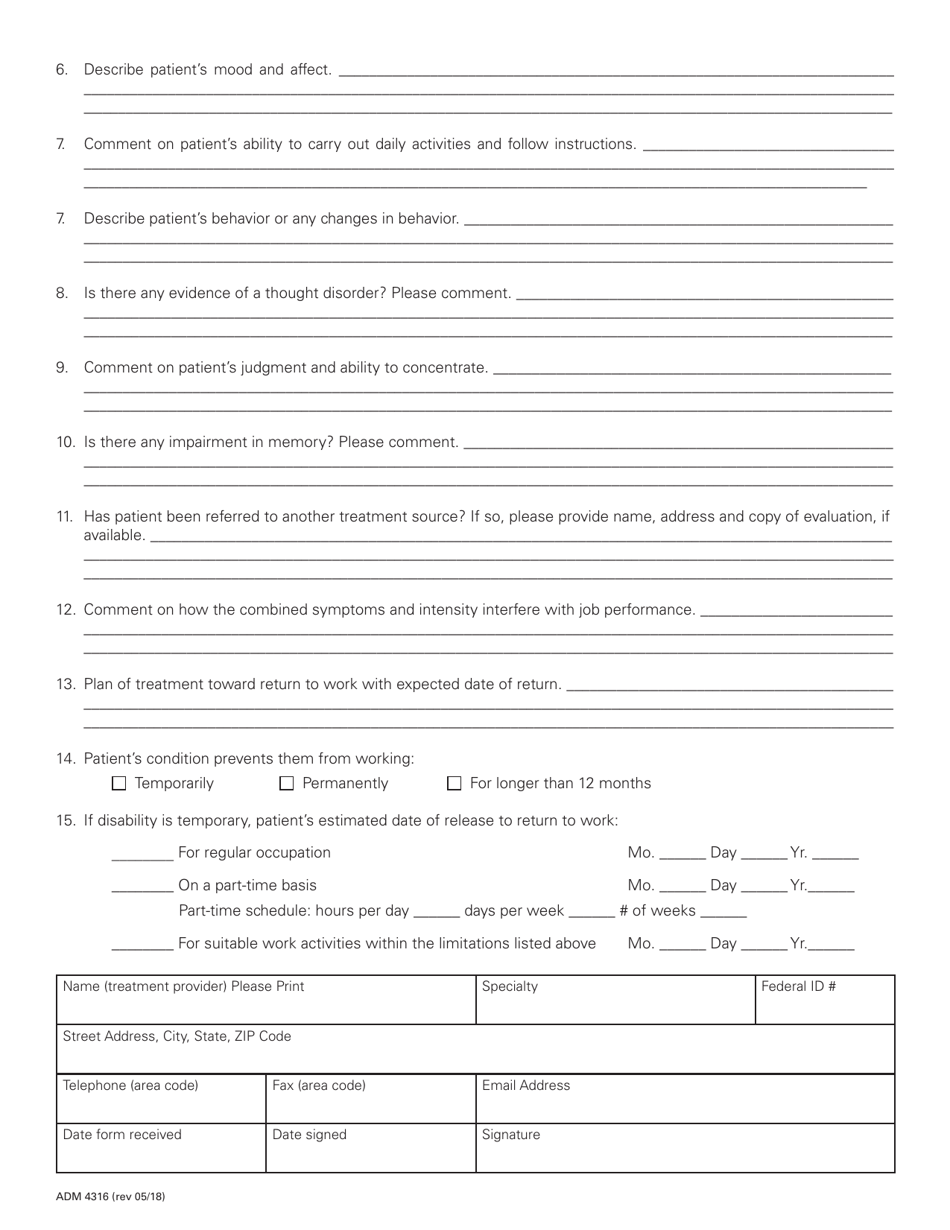
Form ADM4316
for the current year.
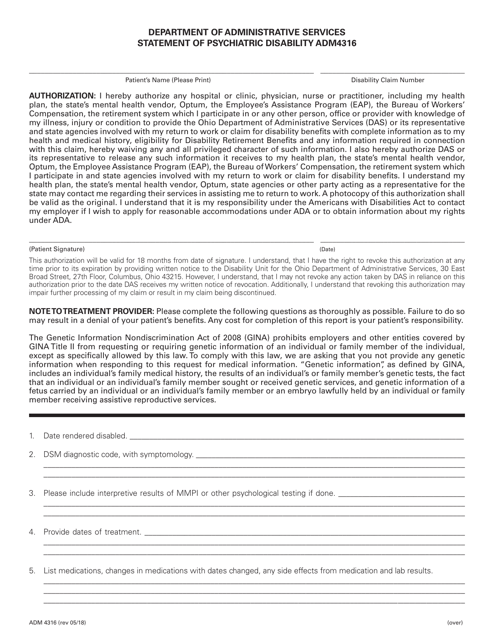
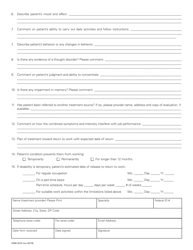
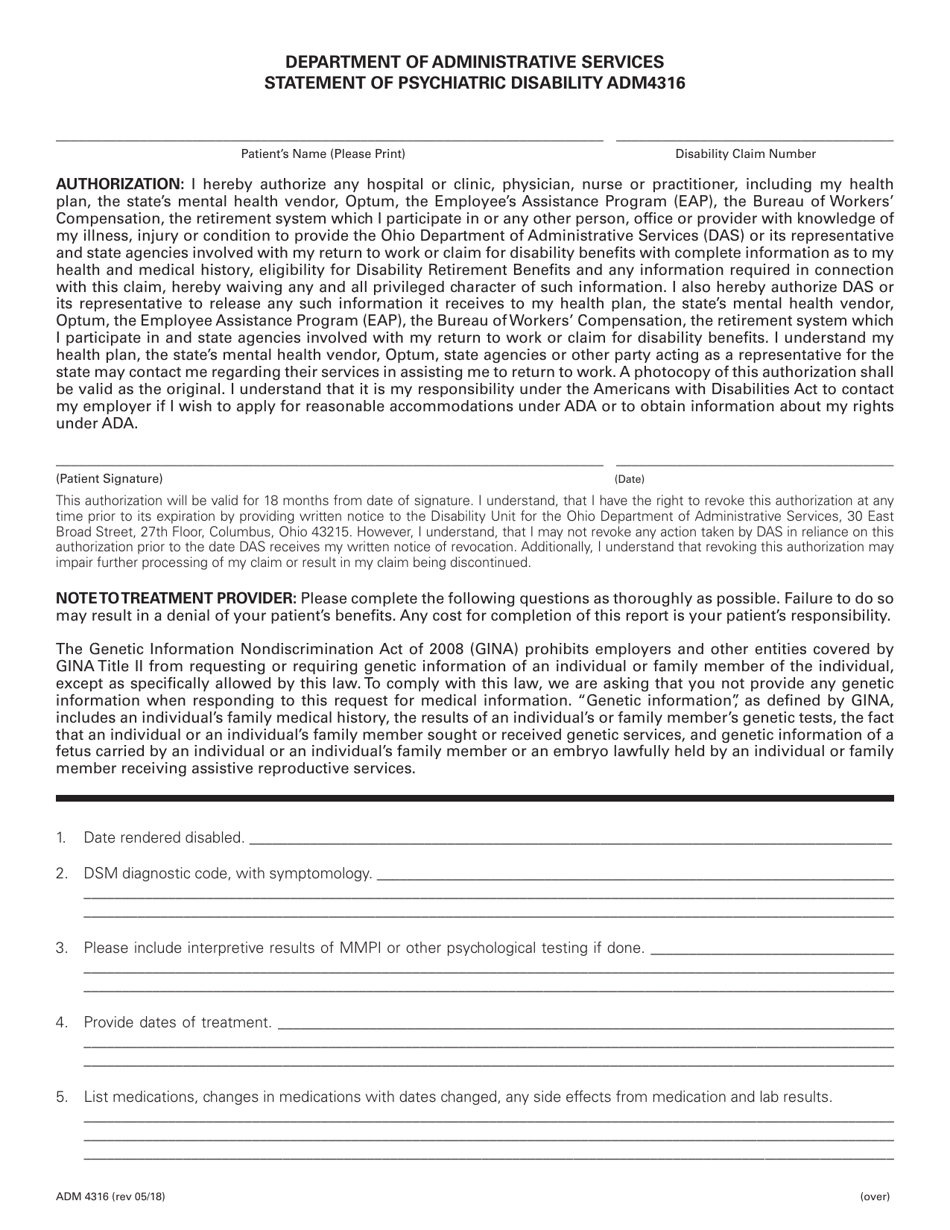
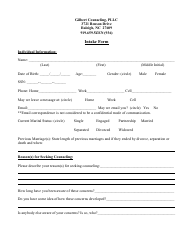
Form ADM4316 Statement of Psychiatric Disability - Ohio
What Is Form ADM4316?
This is a legal form that was released by the Ohio Department of Administrative Services - a government authority operating within Ohio. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is the ADM4316 Statement of Psychiatric Disability?
A: The ADM4316 Statement of Psychiatric Disability is a form used in Ohio to provide documentation of a psychiatric disability.
Q: Who needs to complete the ADM4316 form?
A: The ADM4316 form needs to be completed by a licensed mental health professional or a qualified medical professional.
Q: What is the purpose of the ADM4316 form?
A: The purpose of the ADM4316 form is to document and certify the presence of a psychiatric disability for individuals seeking disability benefits or accommodations.
Q: How should the ADM4316 form be filled out?
A: The ADM4316 form should be completed by providing accurate and detailed information about the individual's psychiatric disability, including symptoms, diagnosis, treatment, and functional limitations.
Q: Can I use the ADM4316 form for disability claims outside of Ohio?
A: No, the ADM4316 form is specific to Ohio and may not be applicable for disability claims in other states.
Q: Does completing the ADM4316 form guarantee approval of disability benefits?
A: No, the completion of the ADM4316 form is just one aspect of the disability claim process. Approval of disability benefits is determined based on various factors, including medical documentation, functional limitations, and eligibility criteria.
Form Details:
- Released on May 1, 2018;
- The latest edition provided by the Ohio Department of Administrative Services;
- Easy to use and ready to print;
- Quick to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of Form ADM4316 by clicking the link below or browse more documents and templates provided by the Ohio Department of Administrative Services.