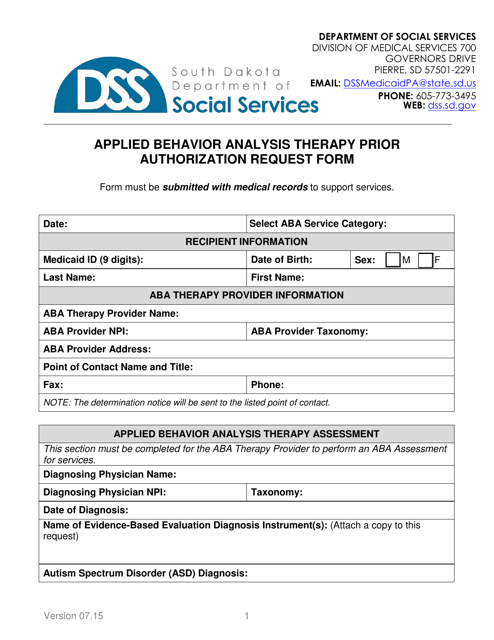
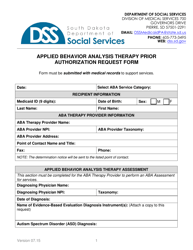
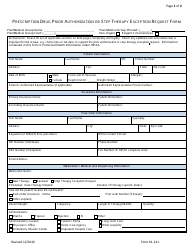
Applied Behavior Analysis Therapy Prior Authorization Request Form - South Dakota
Applied Behavior Analysis Therapy Prior Authorization Request Form is a legal document that was released by the South Dakota Department of Social Services - a government authority operating within South Dakota.
FAQ
Q: What is the Applied Behavior Analysis Therapy Prior Authorization Request Form?
A: The Applied Behavior Analysis Therapy Prior Authorization Request Form is a form used in South Dakota to request prior authorization for Applied Behavior Analysis (ABA) therapy.
Q: What is Applied Behavior Analysis (ABA) therapy?
A: Applied Behavior Analysis (ABA) therapy is a type of therapy that is used to treat individuals with autism spectrum disorder (ASD) or other developmental disorders. It focuses on improving social, communication, and behavioral skills through the use of positive reinforcement and behavioral interventions.
Q: Why is prior authorization required for ABA therapy?
A: Prior authorization is required for ABA therapy to ensure that it is medically necessary and appropriate for the individual receiving the therapy. It helps to prevent unnecessary costs and ensure that resources are allocated efficiently.
Q: Who can submit the prior authorization request?
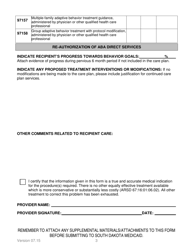
A: The prior authorization request can be submitted by the individual's healthcare provider, such as a physician or licensed psychologist, who is overseeing the ABA therapy.
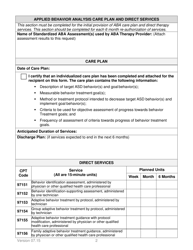
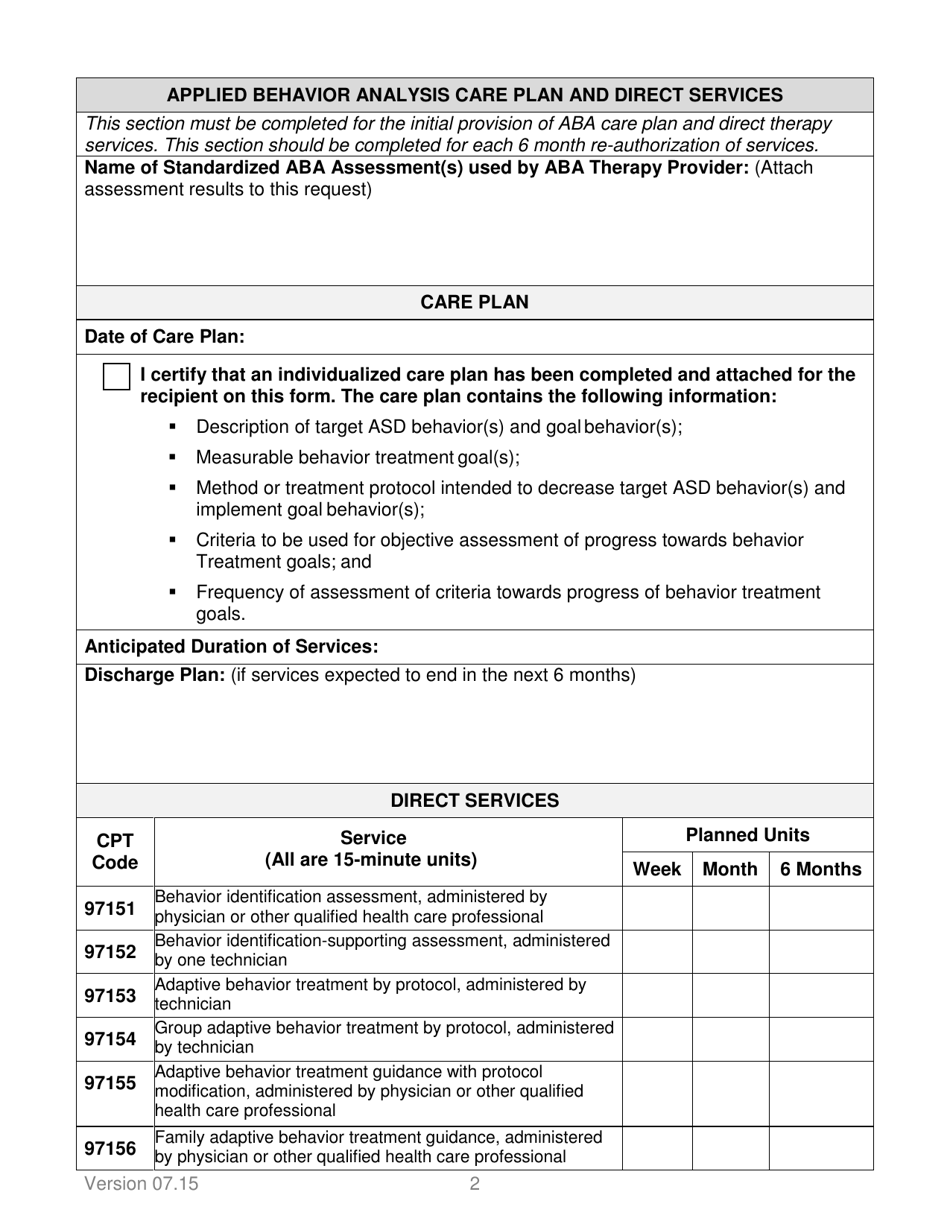
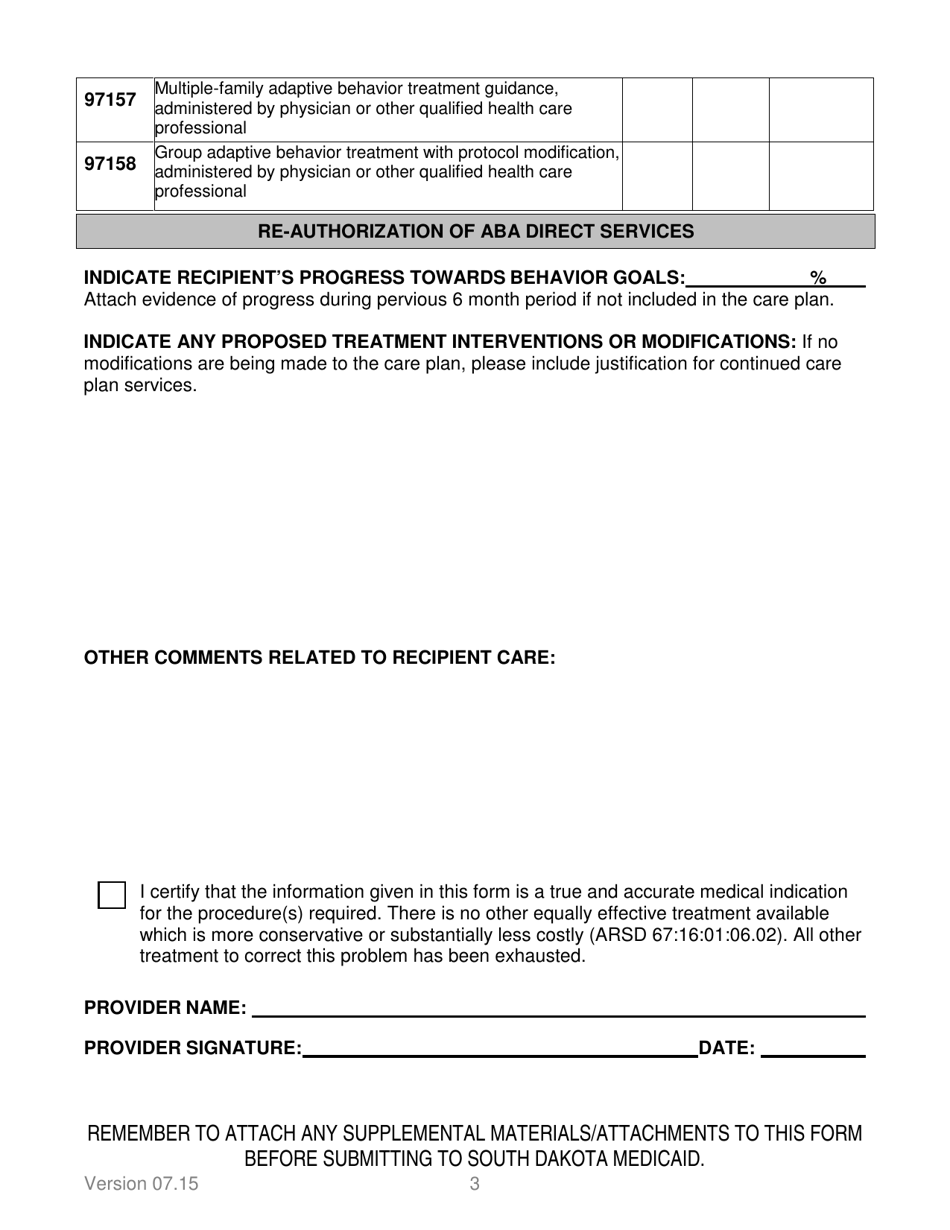
Q: What information is needed on the prior authorization request form?
A: The prior authorization request form typically requires information such as the individual's diagnosis, treatment plan, proposed number of therapy sessions, and supporting documentation from the healthcare provider.
Q: How long does the prior authorization process take?
A: The length of the prior authorization process can vary, but it typically takes a few days to a few weeks for a decision to be made. It is important to submit the request well in advance of the desired start date for ABA therapy.
Q: What happens after the prior authorization request is submitted?
A: After the prior authorization request is submitted, the insurance company will review the request and determine whether to approve or deny the request. The healthcare provider and the individual will be notified of the decision.
Q: What can I do if the prior authorization request is denied?
A: If the prior authorization request is denied, it is important to review the denial letter and understand the reason for the denial. In some cases, the denial can be appealed with additional supporting documentation or an explanation of why the therapy is medically necessary.
Q: Is ABA therapy covered by insurance?
A: Many insurance plans provide coverage for ABA therapy, but coverage can vary. It is important to check with the individual's insurance company to determine their specific coverage and any requirements for prior authorization.
Form Details:
- Released on July 1, 2015;
- The latest edition currently provided by the South Dakota Department of Social Services;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of the form by clicking the link below or browse more documents and templates provided by the South Dakota Department of Social Services.