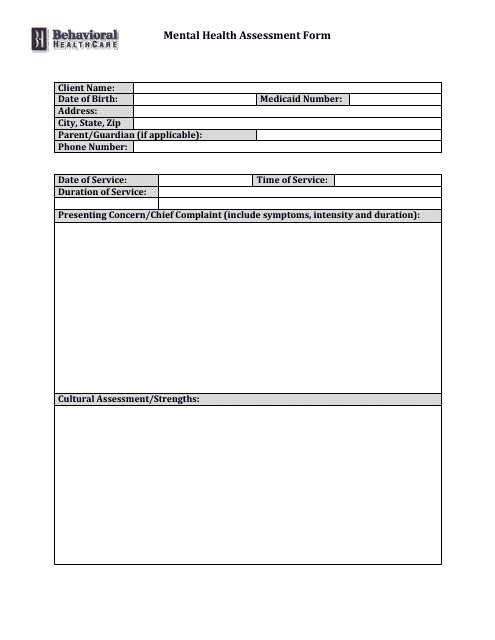
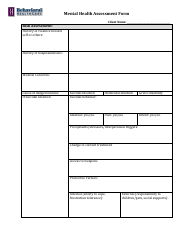
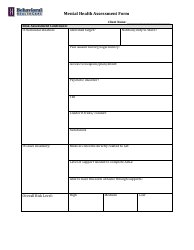
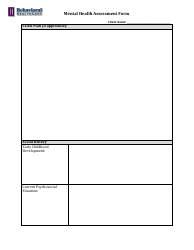
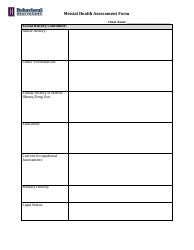
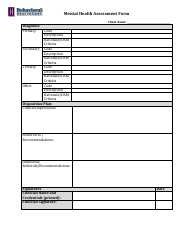
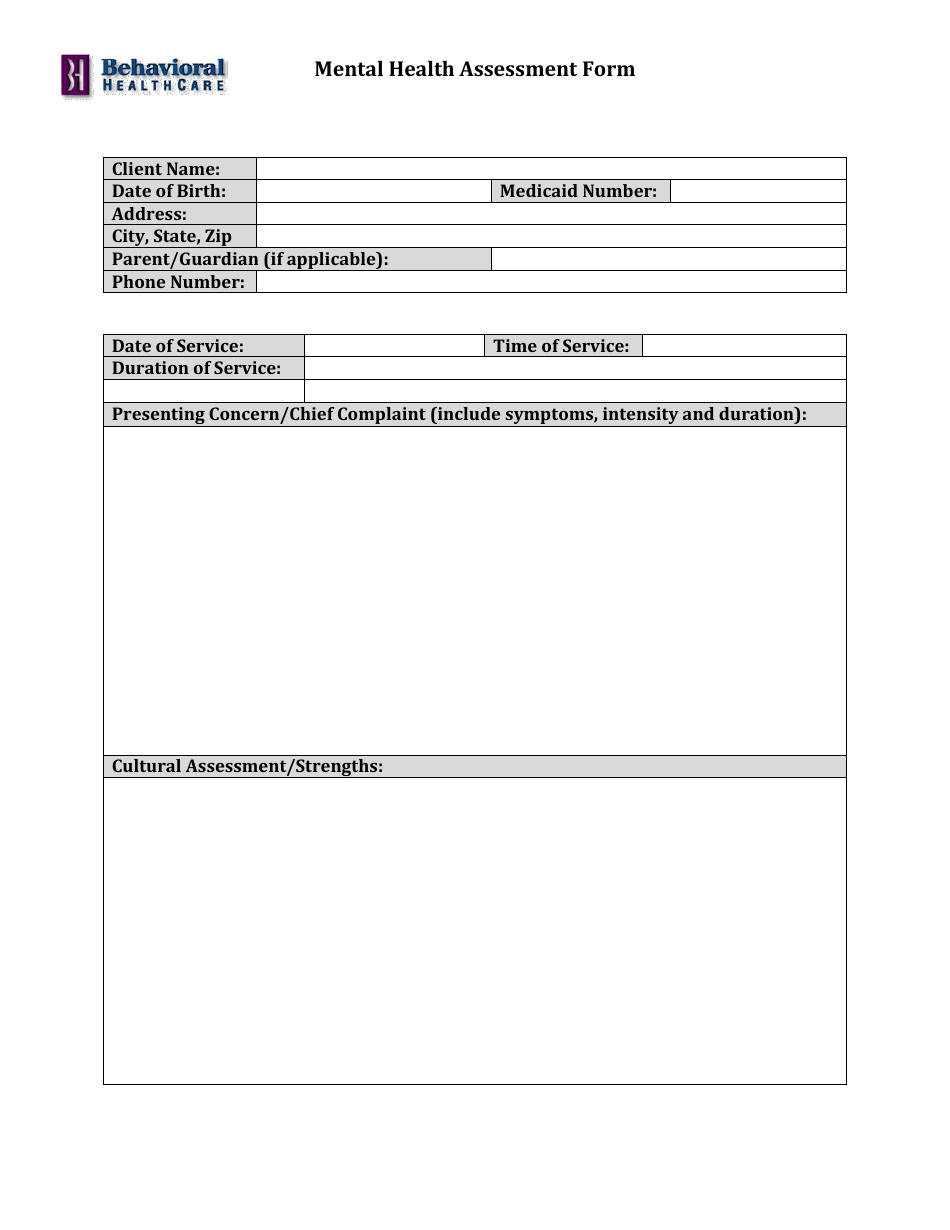
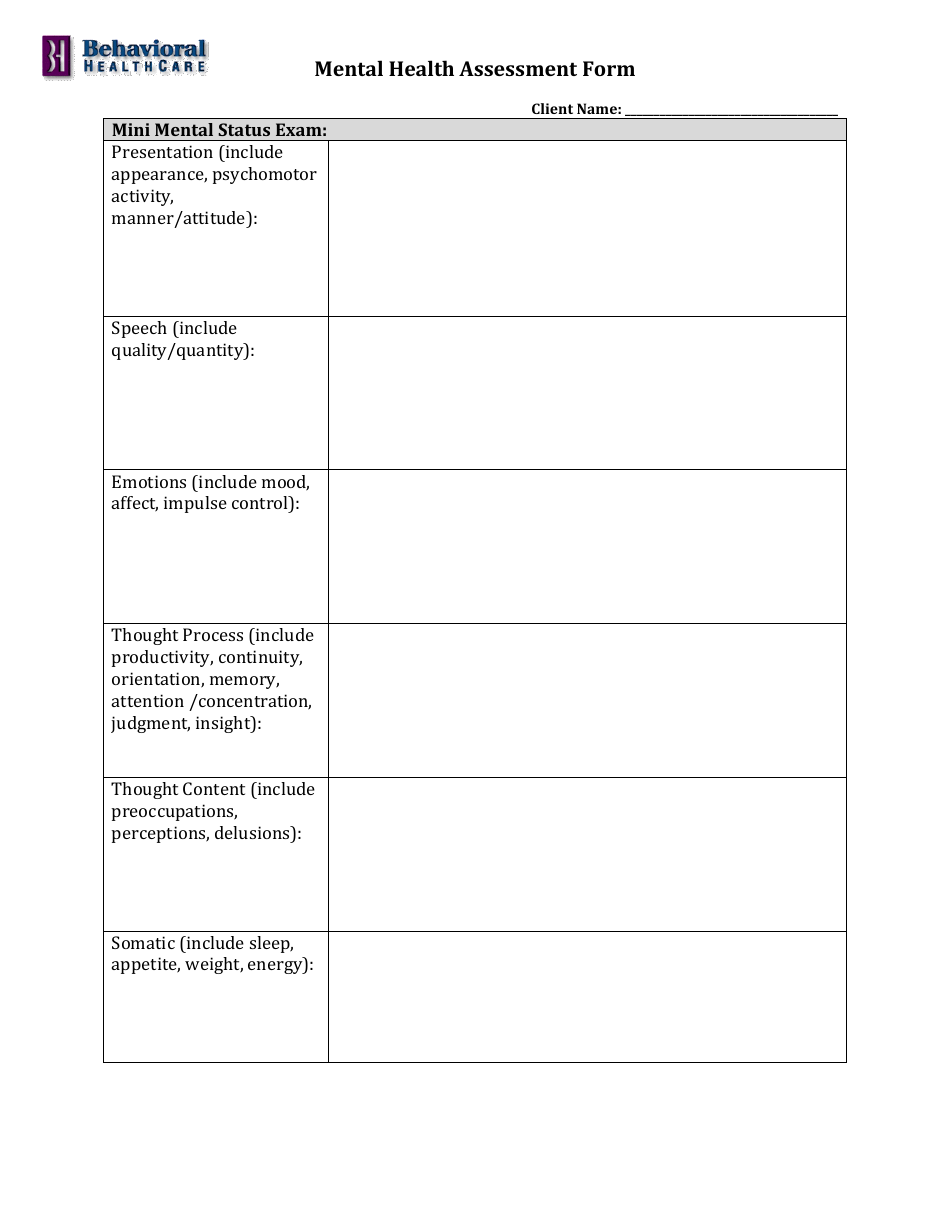
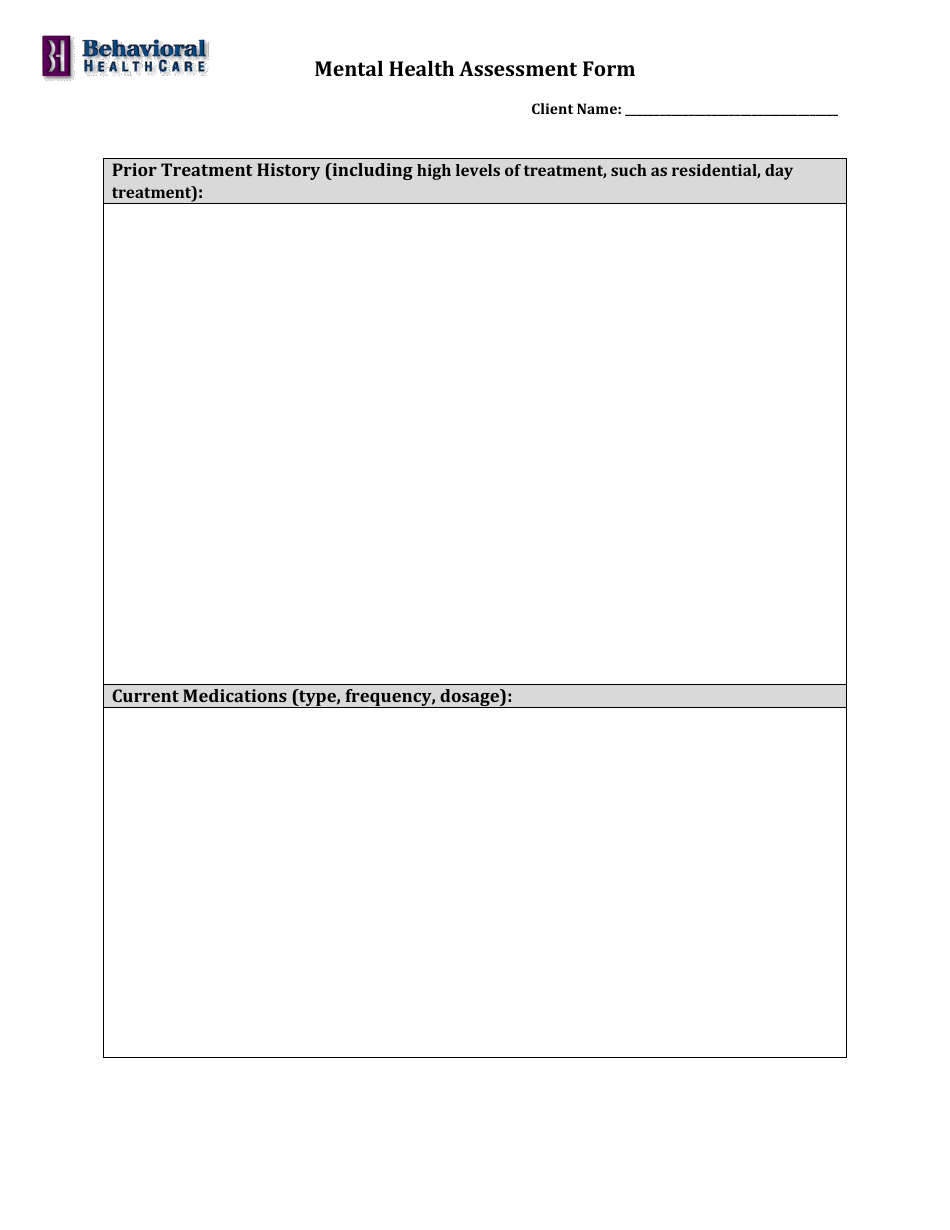
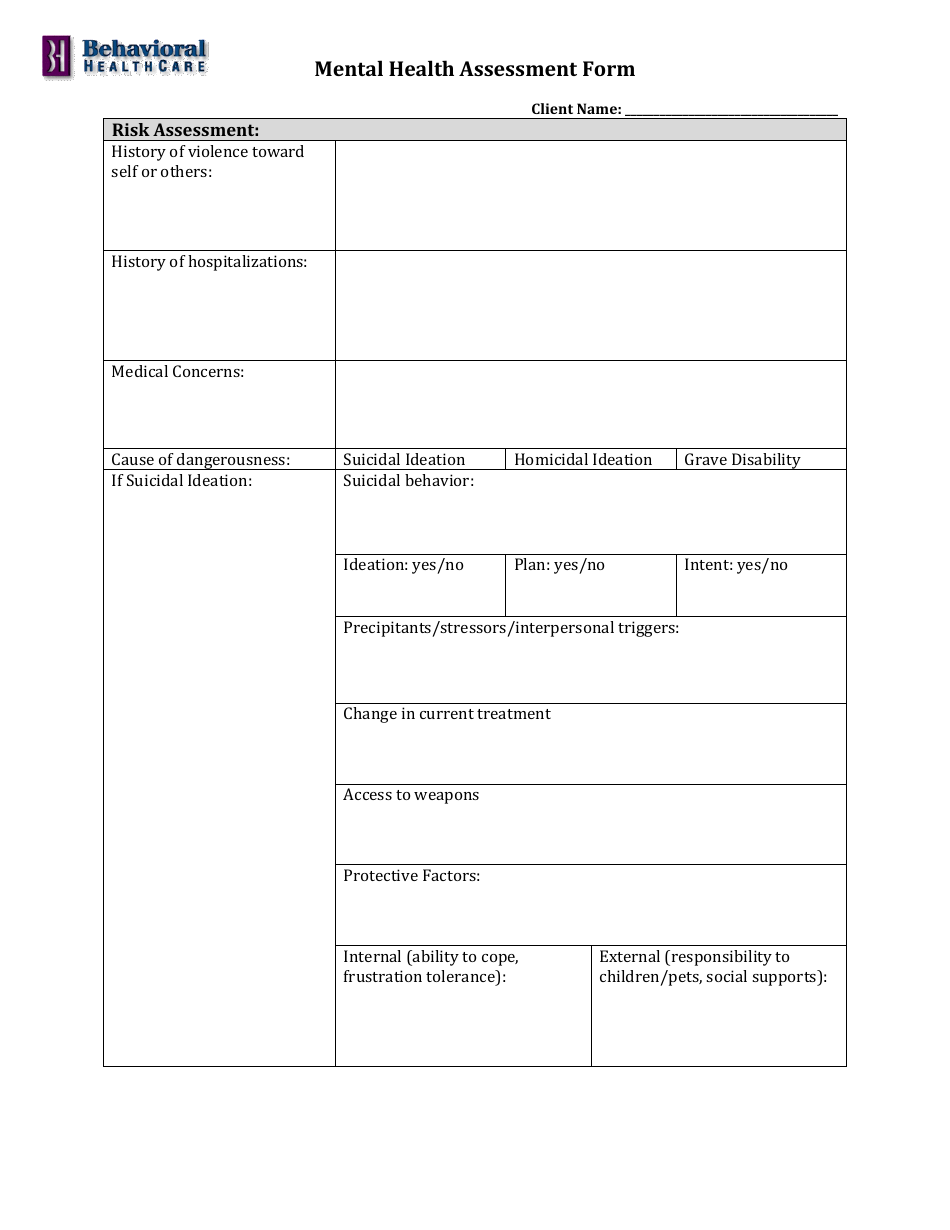
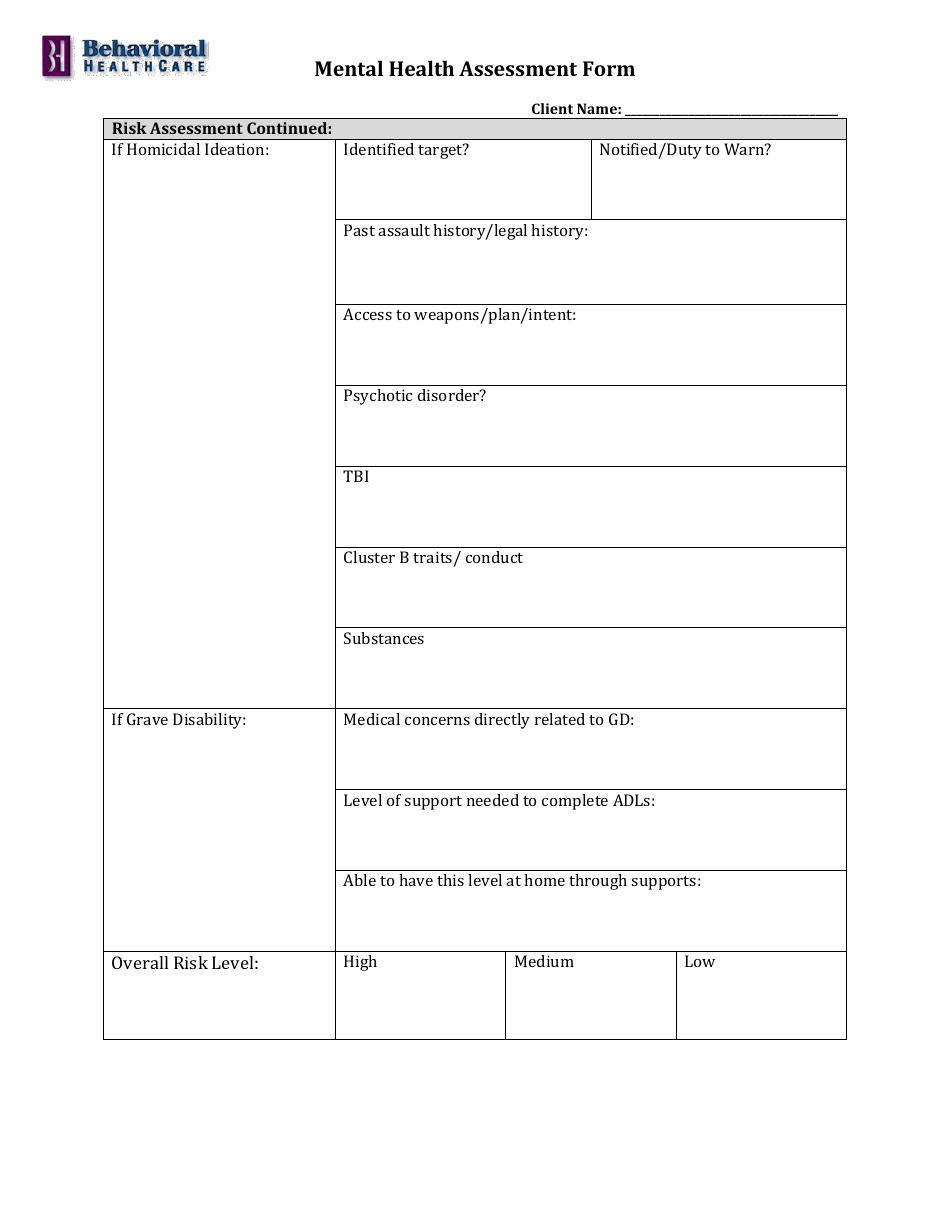
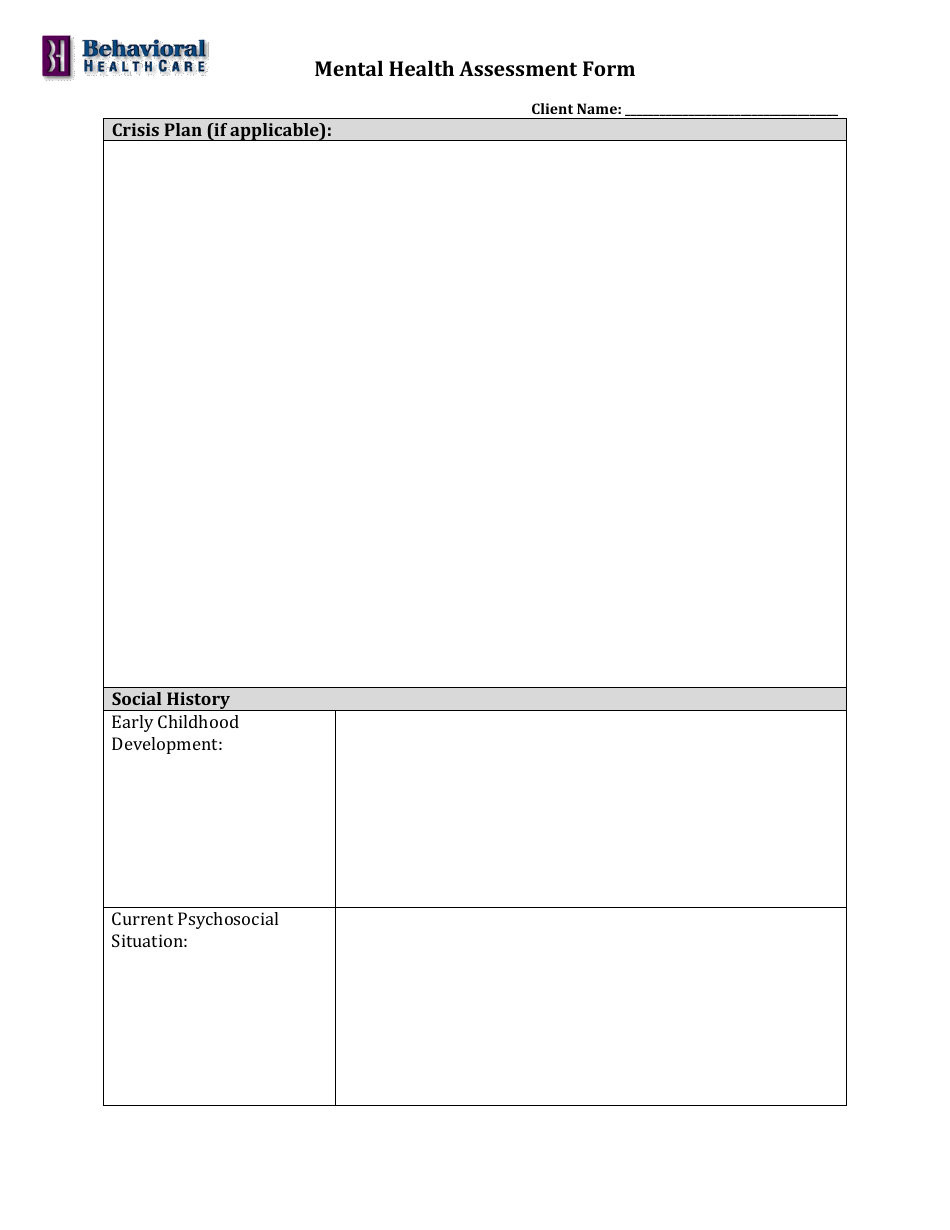
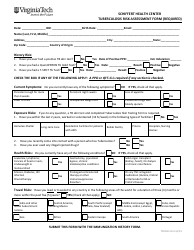
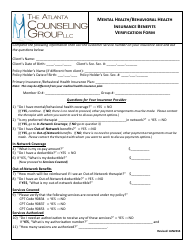
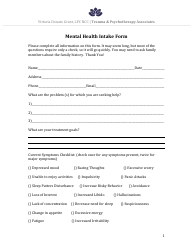
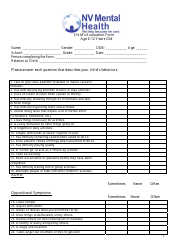
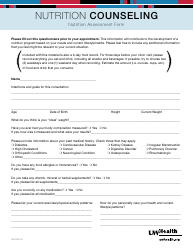
Mental Health Assessment Form - Behavioral Healthcare
The Mental Health Assessment Form - Behavioral Healthcare is used to evaluate an individual's mental health and provide necessary information for their treatment and care. It helps healthcare providers assess symptoms, challenges, and overall mental well-being.
The individual seeking mental health assessment typically fills out the form.
FAQ
Q: What is a mental health assessment form?
A: A mental health assessment form is a tool used in behavioral healthcare to gather information about an individual's mental health and well-being.
Q: Why is a mental health assessment important?
A: A mental health assessment is important as it helps healthcare providers evaluate an individual's mental health, identify any potential issues or disorders, and determine appropriate treatment options.
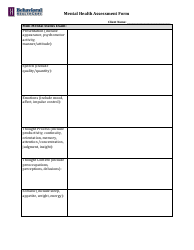
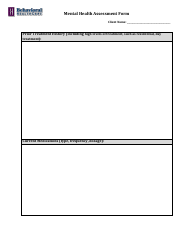
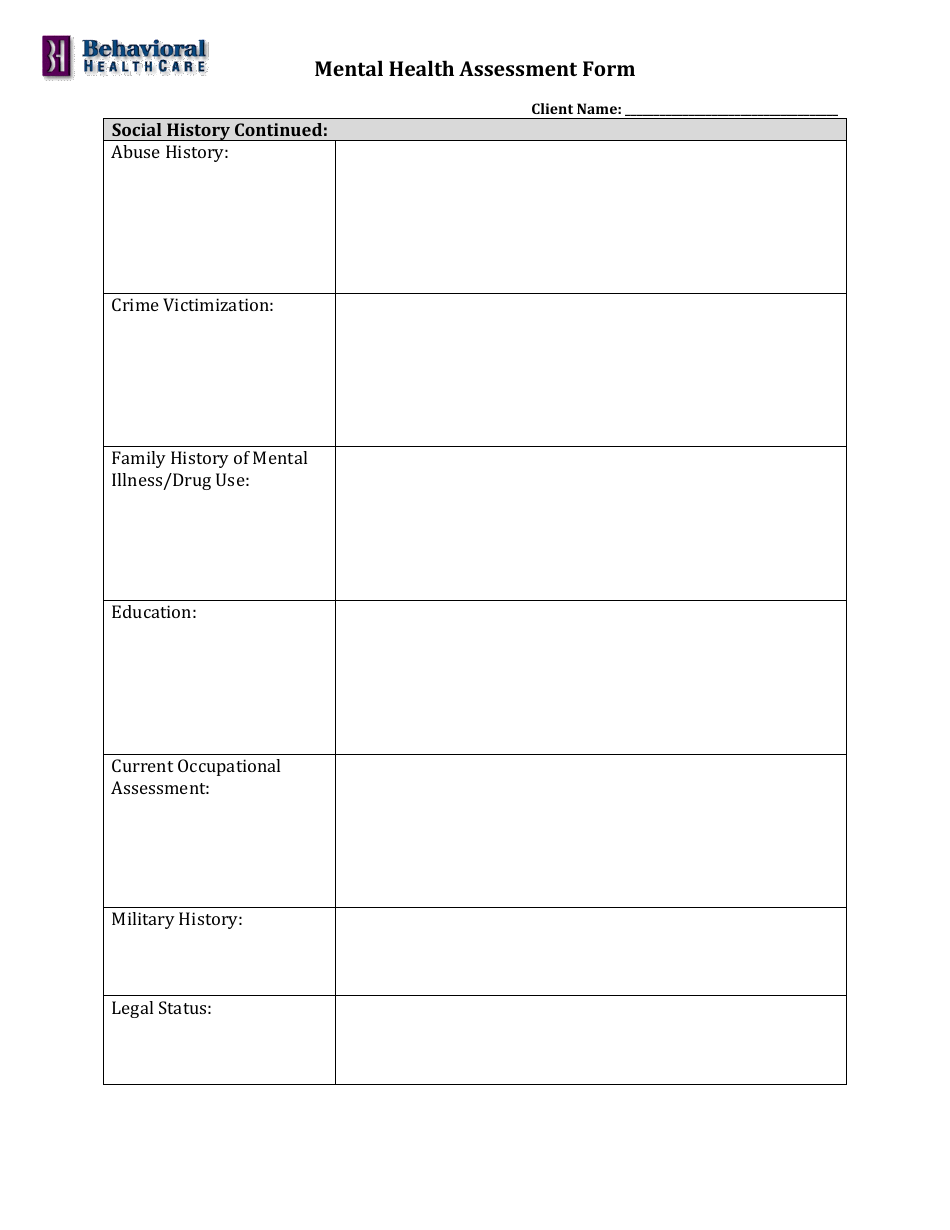
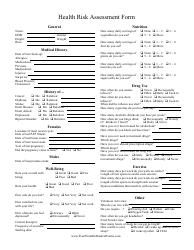
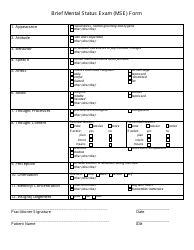
Q: What information is typically included in a mental health assessment form?
A: A mental health assessment form usually includes questions about an individual's personal background, medical history, current symptoms, and any previous mental health treatments.
Q: Who completes a mental health assessment form?
A: A mental health assessment form is typically completed by the individual seeking mental health services, with guidance and assistance from a healthcare provider.
Q: How long does a mental health assessment take?
A: The duration of a mental health assessment can vary depending on the complexity of an individual's situation, but it generally takes around 1-2 hours to complete.
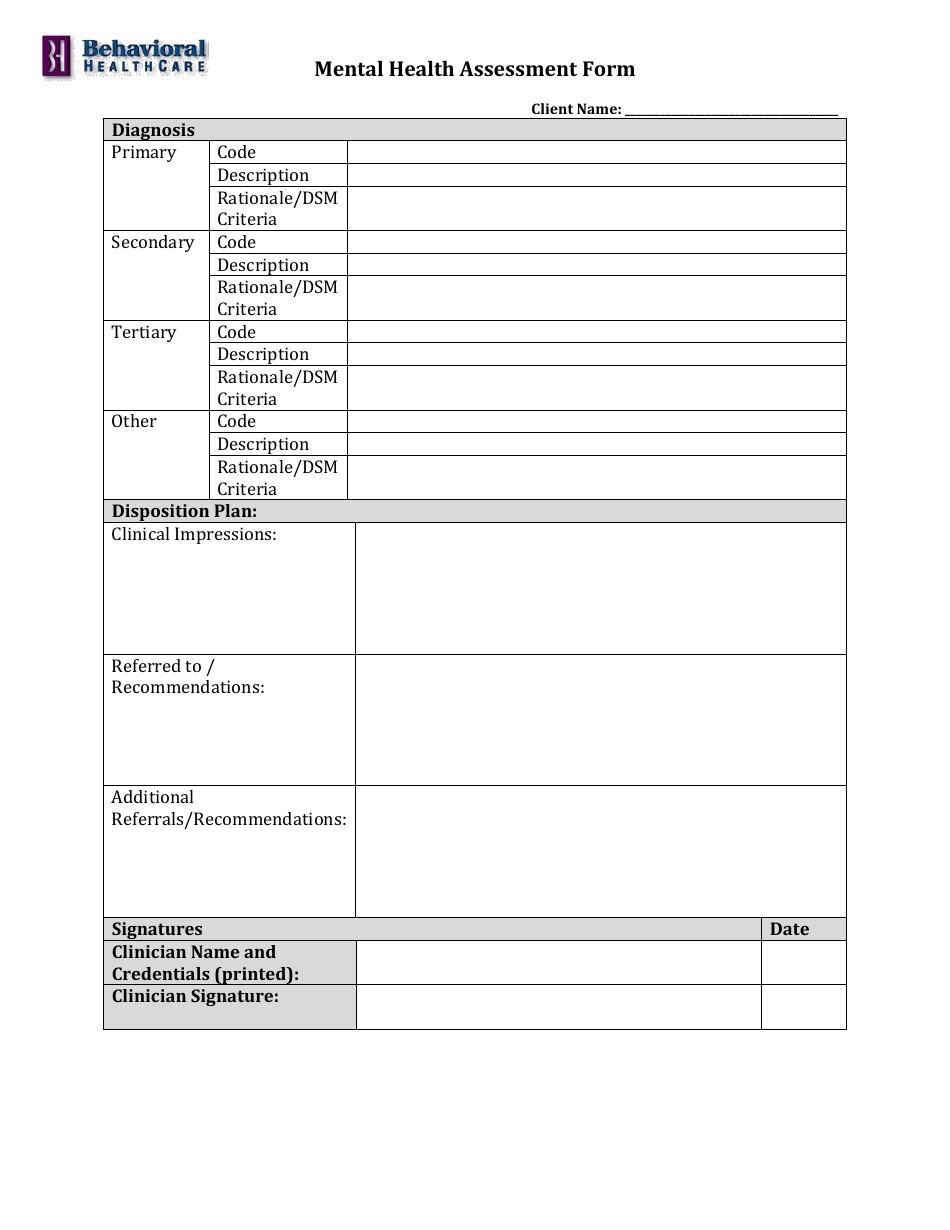
Q: Can a mental health assessment form diagnose mental disorders?
A: No, a mental health assessment form alone cannot diagnose mental disorders. It helps gather information for healthcare providers, who use their professional judgment to make a diagnosis.
Q: Is a mental health assessment confidential?
A: Yes, mental health assessments are treated as confidential and protected by privacy laws. The information provided is only shared with authorized individuals involved in the individual's care.