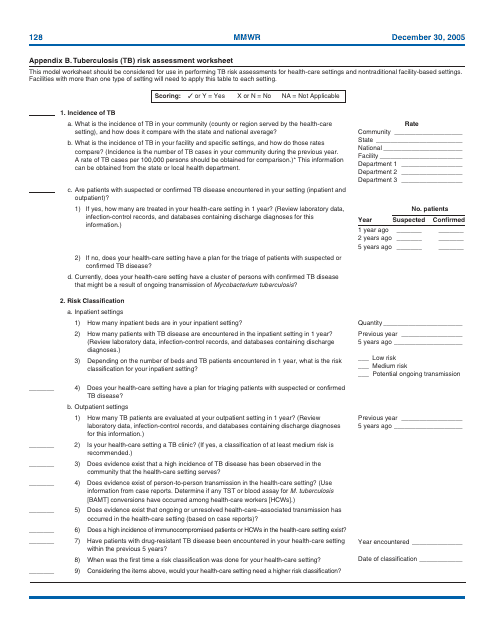
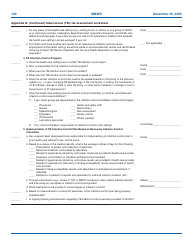
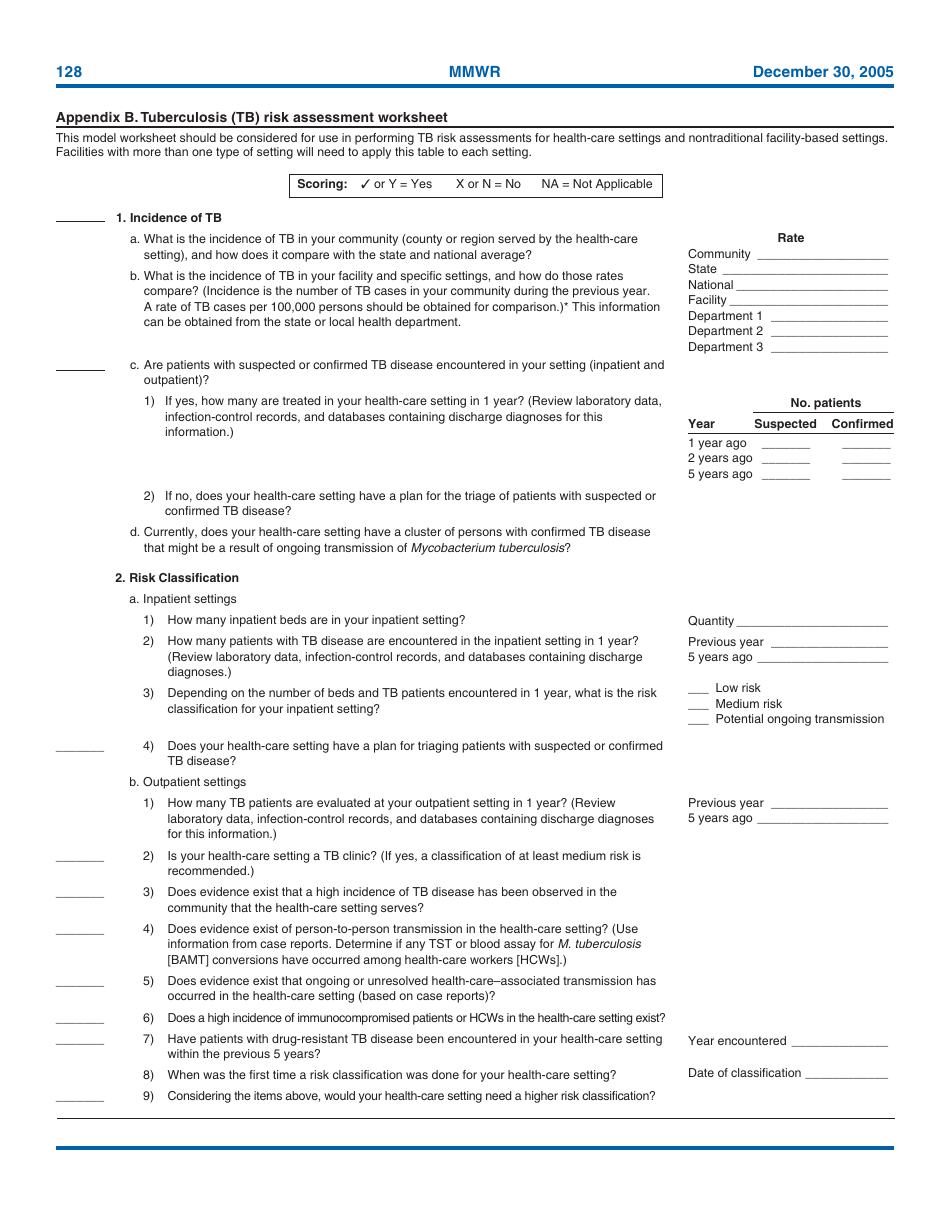
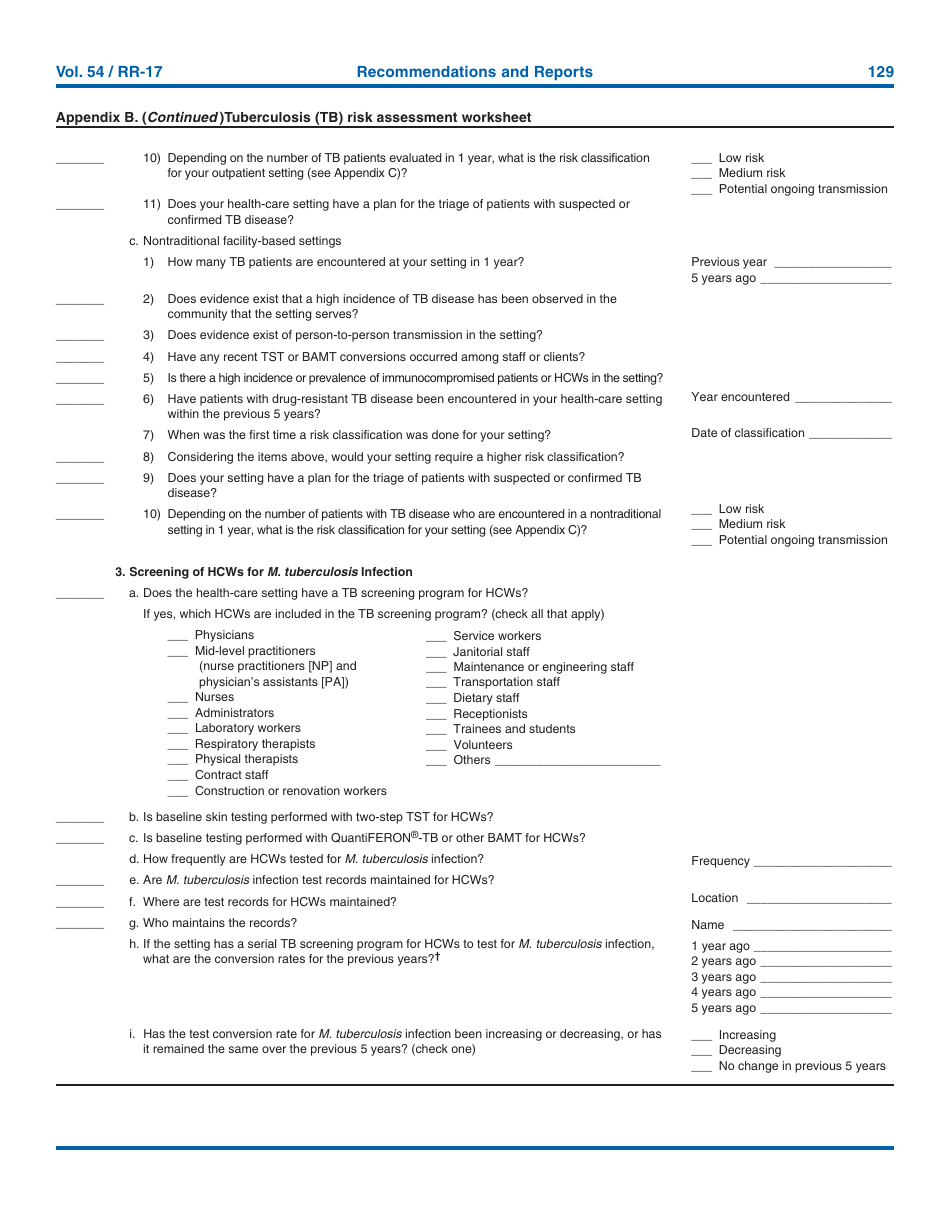
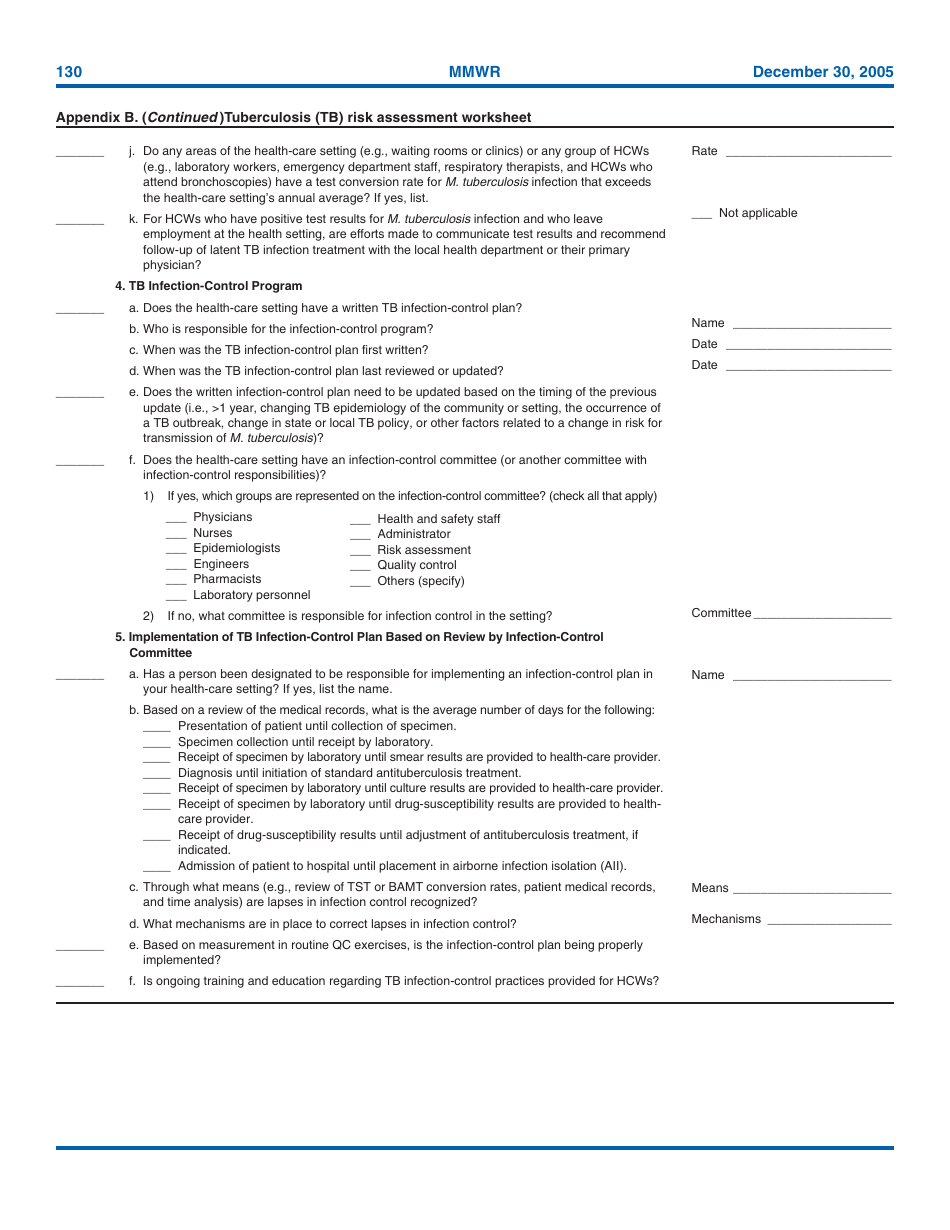
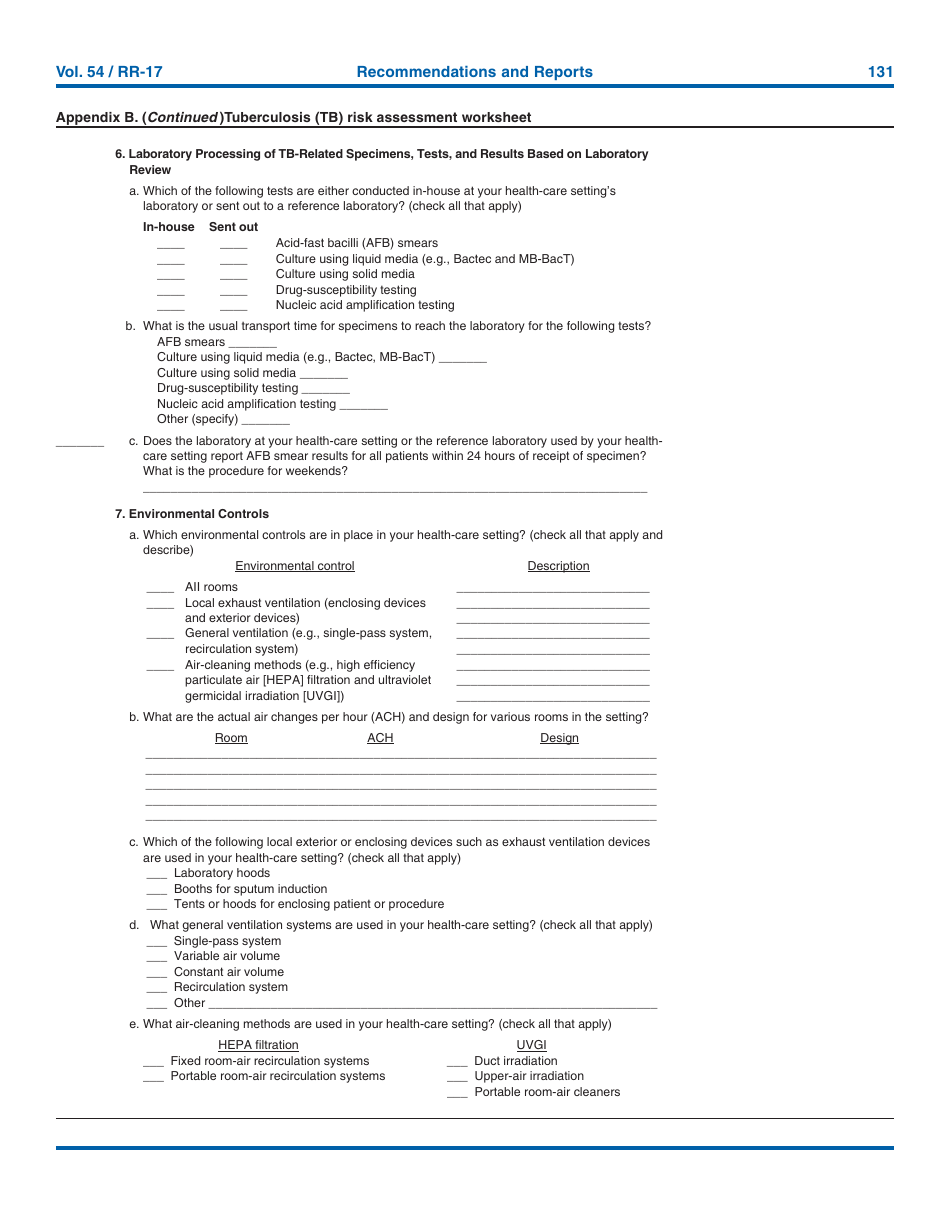
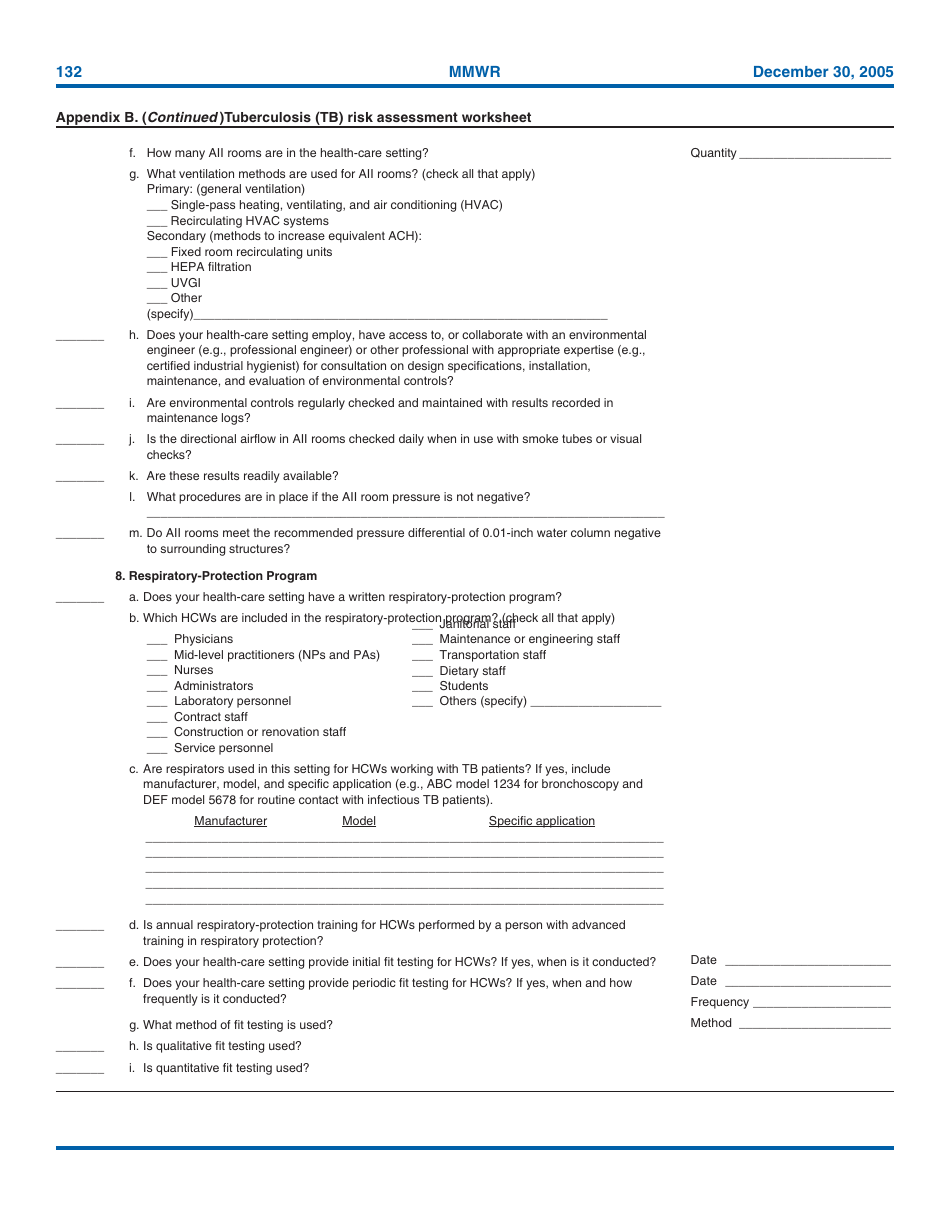
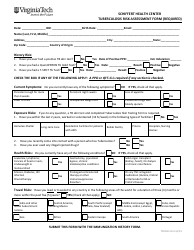
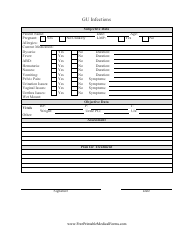
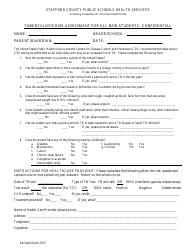
Tuberculosis Risk Assessment Worksheet
The Tuberculosis Risk Assessment Worksheet is used by healthcare professionals to assess an individual's risk of developing tuberculosis (TB). It helps determine if further diagnostic testing or preventive measures are necessary.
The Tuberculosis Risk Assessment Worksheet is typically filed by healthcare providers or medical professionals who are responsible for assessing the risk of tuberculosis in individuals.
FAQ
Q: What is a Tuberculosis Risk Assessment Worksheet?
A: A Tuberculosis Risk Assessment Worksheet is a tool used to assess an individual's risk of developing tuberculosis.
Q: How is a Tuberculosis Risk Assessment Worksheet used?
A: A Tuberculosis Risk Assessment Worksheet is used by healthcare professionals to evaluate the likelihood of a person having tuberculosis based on certain risk factors.
Q: What are the risk factors considered in a Tuberculosis Risk Assessment Worksheet?
A: Risk factors considered in a Tuberculosis Risk Assessment Worksheet may include recent travel to high-risk areas, exposure to people with tuberculosis, and certain medical conditions that weaken the immune system.
Q: Why is a Tuberculosis Risk Assessment Worksheet important?
A: A Tuberculosis Risk Assessment Worksheet is important as it helps healthcare professionals determine if an individual needs further testing or treatment for tuberculosis.
Q: Can a Tuberculosis Risk Assessment Worksheet diagnose tuberculosis?
A: No, a Tuberculosis Risk Assessment Worksheet cannot diagnose tuberculosis. It is simply a tool to evaluate the risk of having the disease.