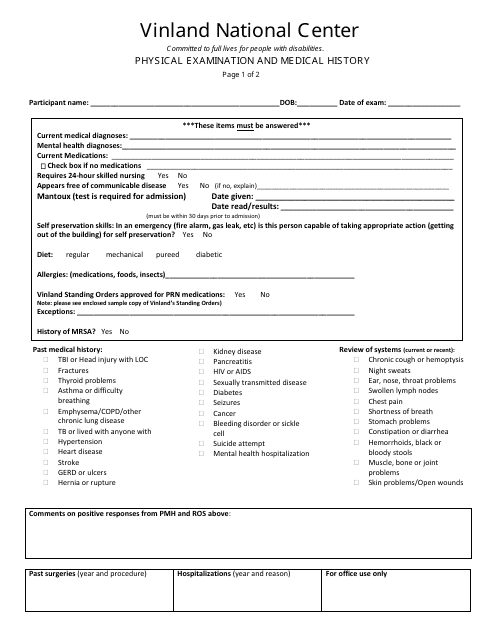
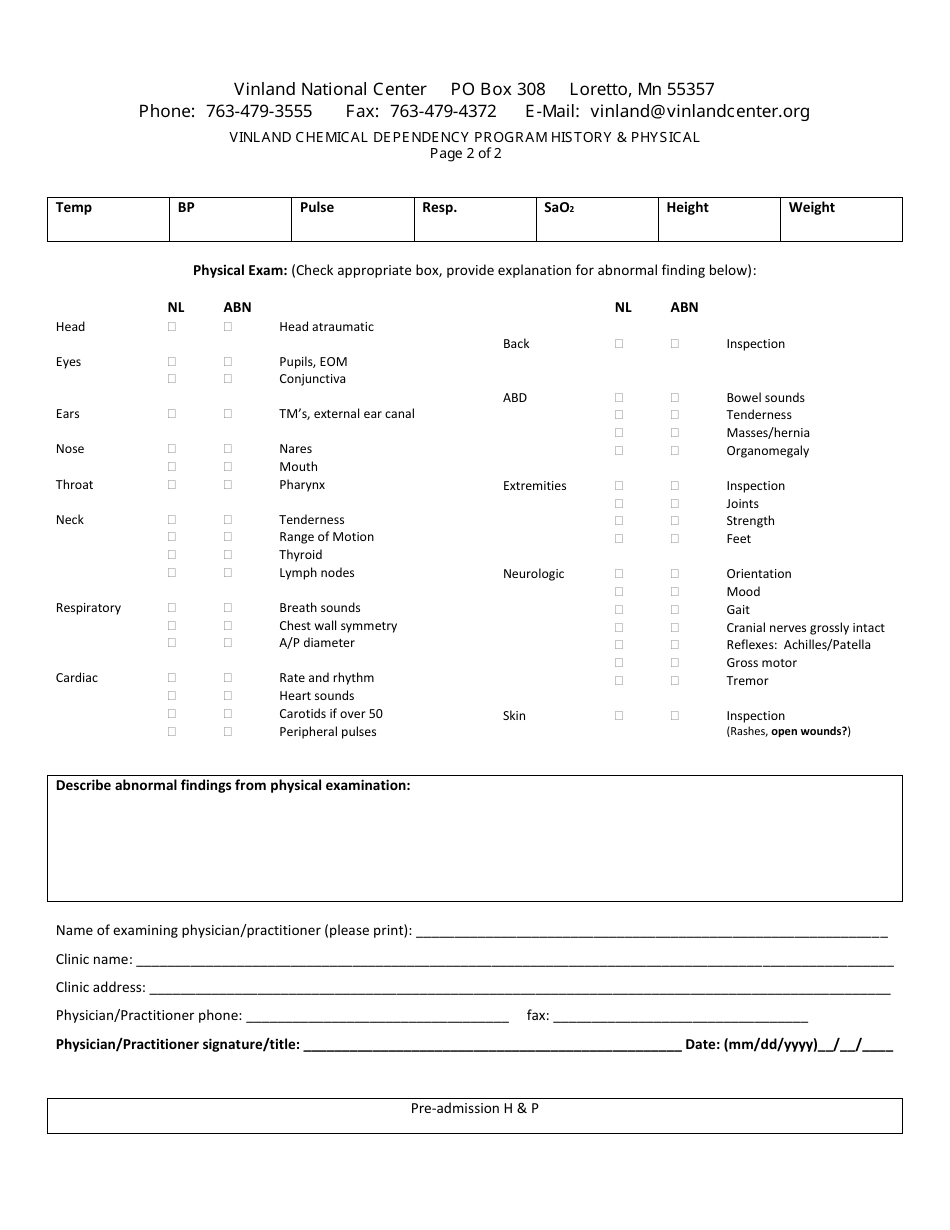
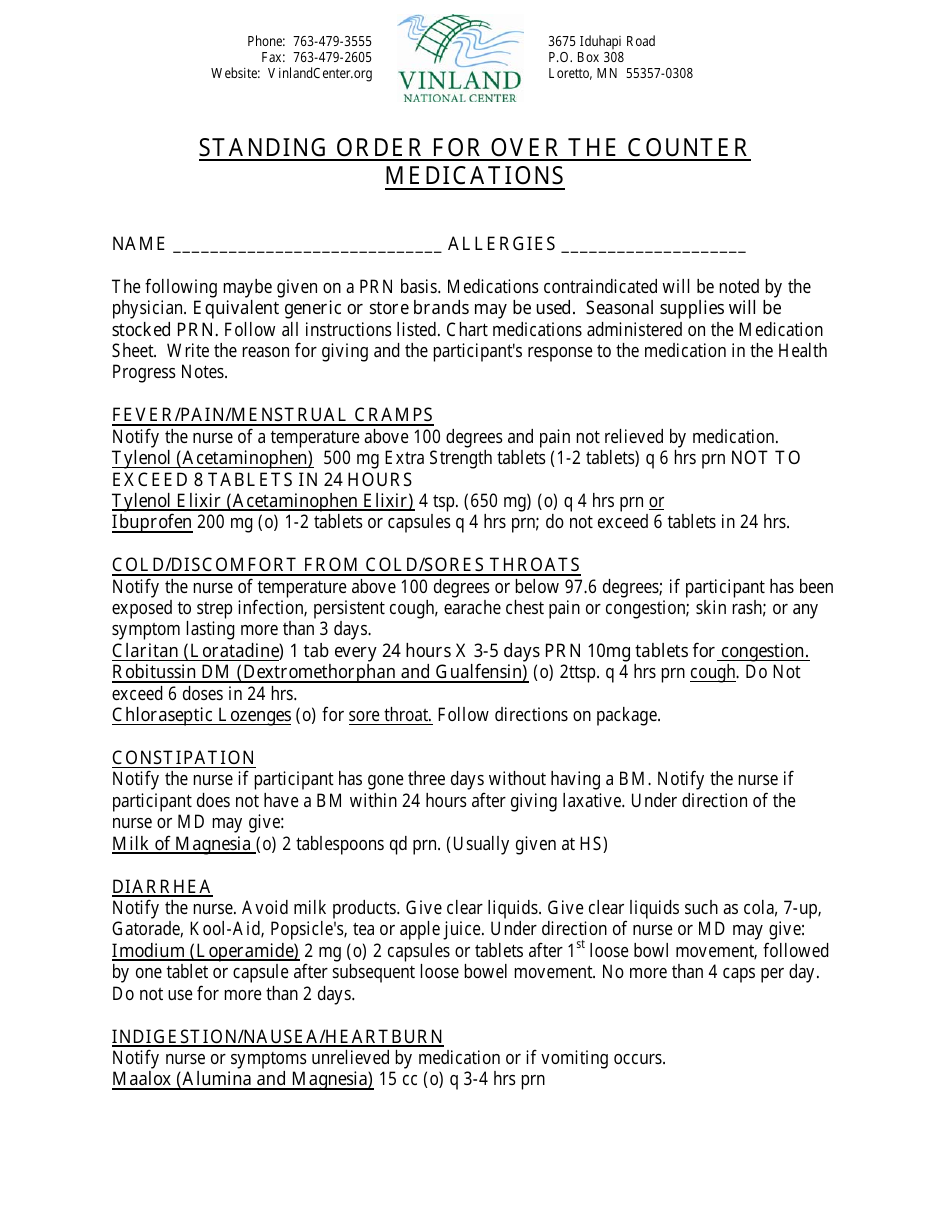
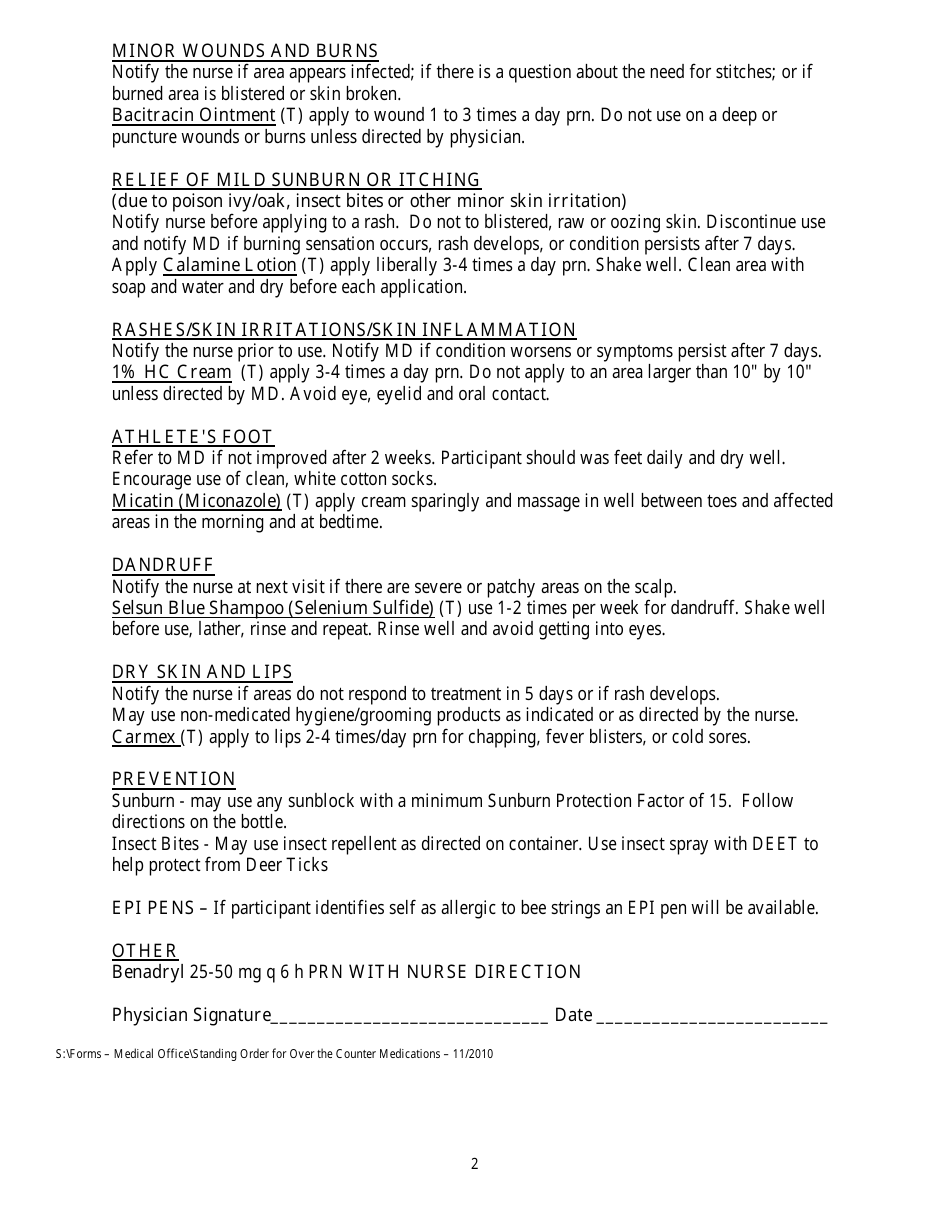
Physical Examination and Medical History Form - Vinland National Center
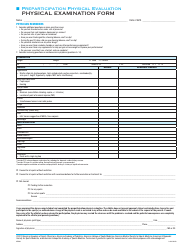
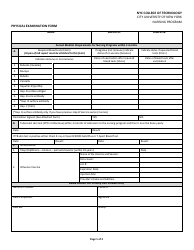
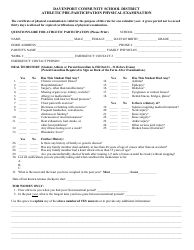
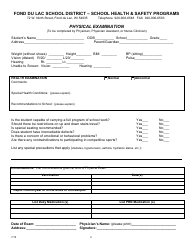
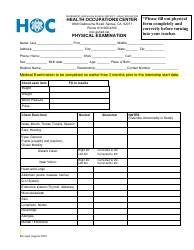
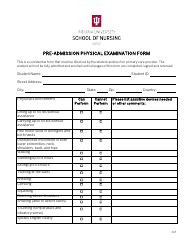
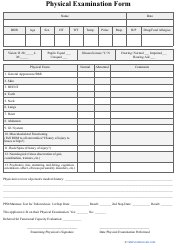
The Physical Examination and Medical History Form is used by the Vinland National Center for individuals to provide information about their medical history and undergo a physical examination. This form helps the center evaluate and understand the health status of individuals.
FAQ
Q: What is the purpose of the Physical Examination and Medical History Form at Vinland National Center?
A: The form is used to gather information about a patient's physical condition and medical history at Vinland National Center.
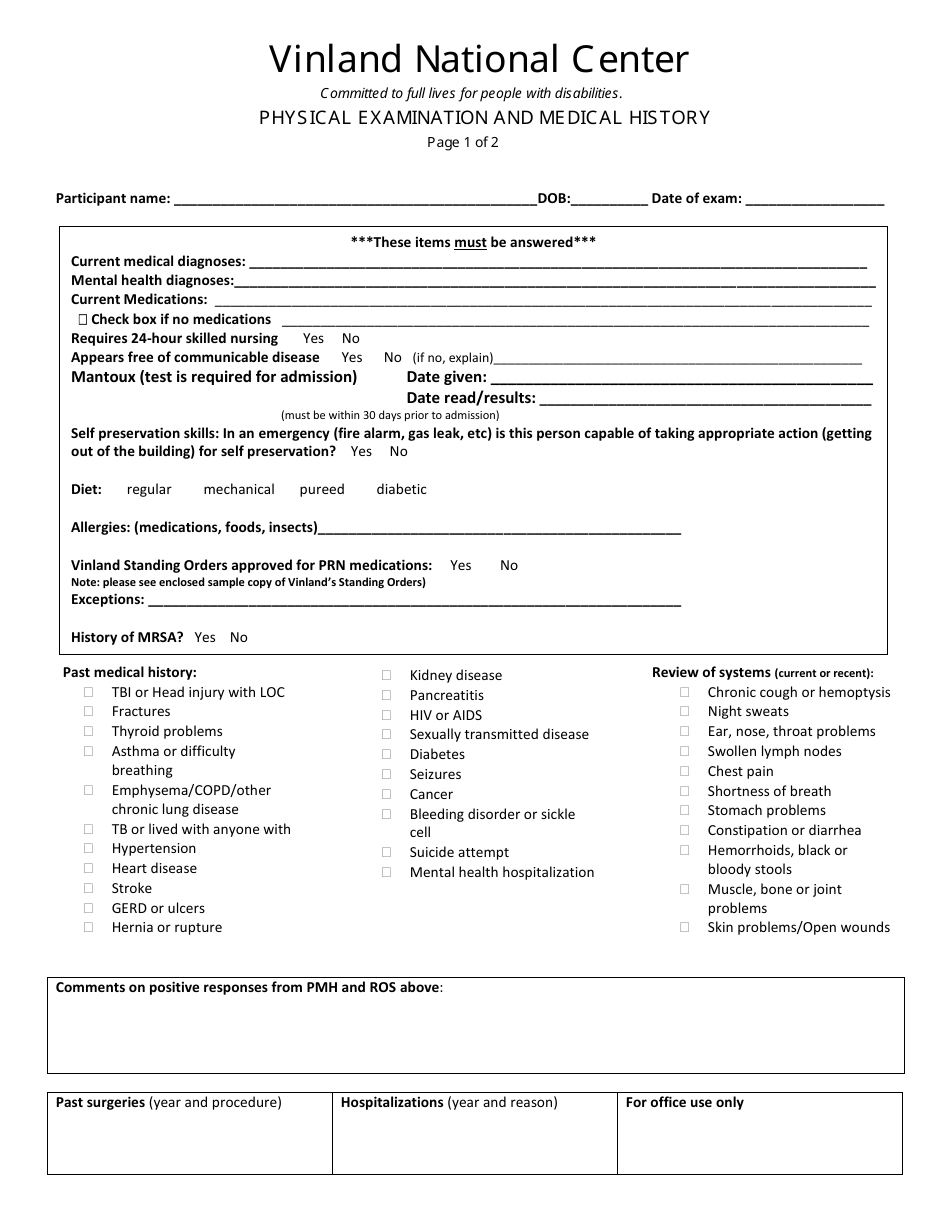
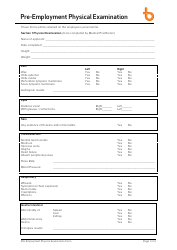
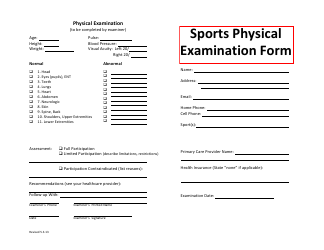
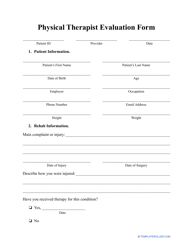
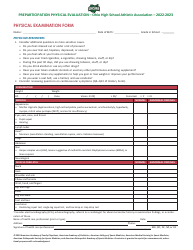
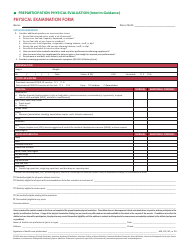
Q: What does the Physical Examination section of the form consist of?
A: The Physical Examination section of the form includes measurements of vital signs, such as blood pressure, heart rate, and body temperature.
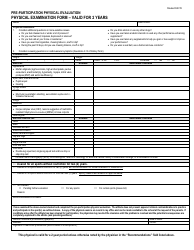
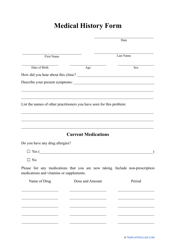
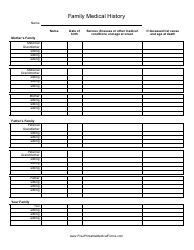
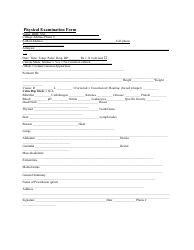
Q: What information is included in the Medical History section of the form?
A: The Medical History section includes questions about previous medical conditions, surgeries, medications, allergies, and family medical history.
Q: Why is it important to provide accurate information on the form?
A: Accurate information is important to ensure proper medical care and to identify any potential risks or contraindications.
Q: Who should fill out the Physical Examination and Medical History Form?
A: The form should be filled out by patients or their legal guardians, with the assistance of healthcare providers if needed.
Q: Is the information on the form kept confidential?
A: Yes, the information on the form is kept confidential and is only shared with healthcare providers involved in the patient's care.
Q: What should I do if I don't understand a question on the form?
A: If you don't understand a question, you can ask for clarification from a healthcare provider or staff member at Vinland National Center.
Q: Is it necessary to bring the form to every appointment at Vinland National Center?
A: Yes, it is recommended to bring the form to every appointment to provide updated information and ensure continuity of care.
Q: Can I make changes or updates to the form after it has been submitted?
A: Yes, you can make changes or updates to the form by notifying a healthcare provider or staff member at Vinland National Center.
Q: How long is the Physical Examination and Medical History Form kept on file at Vinland National Center?
A: The form is typically kept on file for the duration of a patient's treatment at Vinland National Center.