This version of the form is not currently in use and is provided for reference only. Download this version of
the document
for the current year.
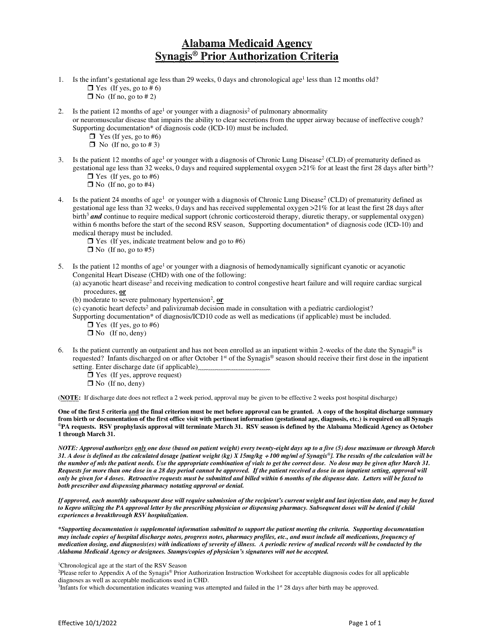
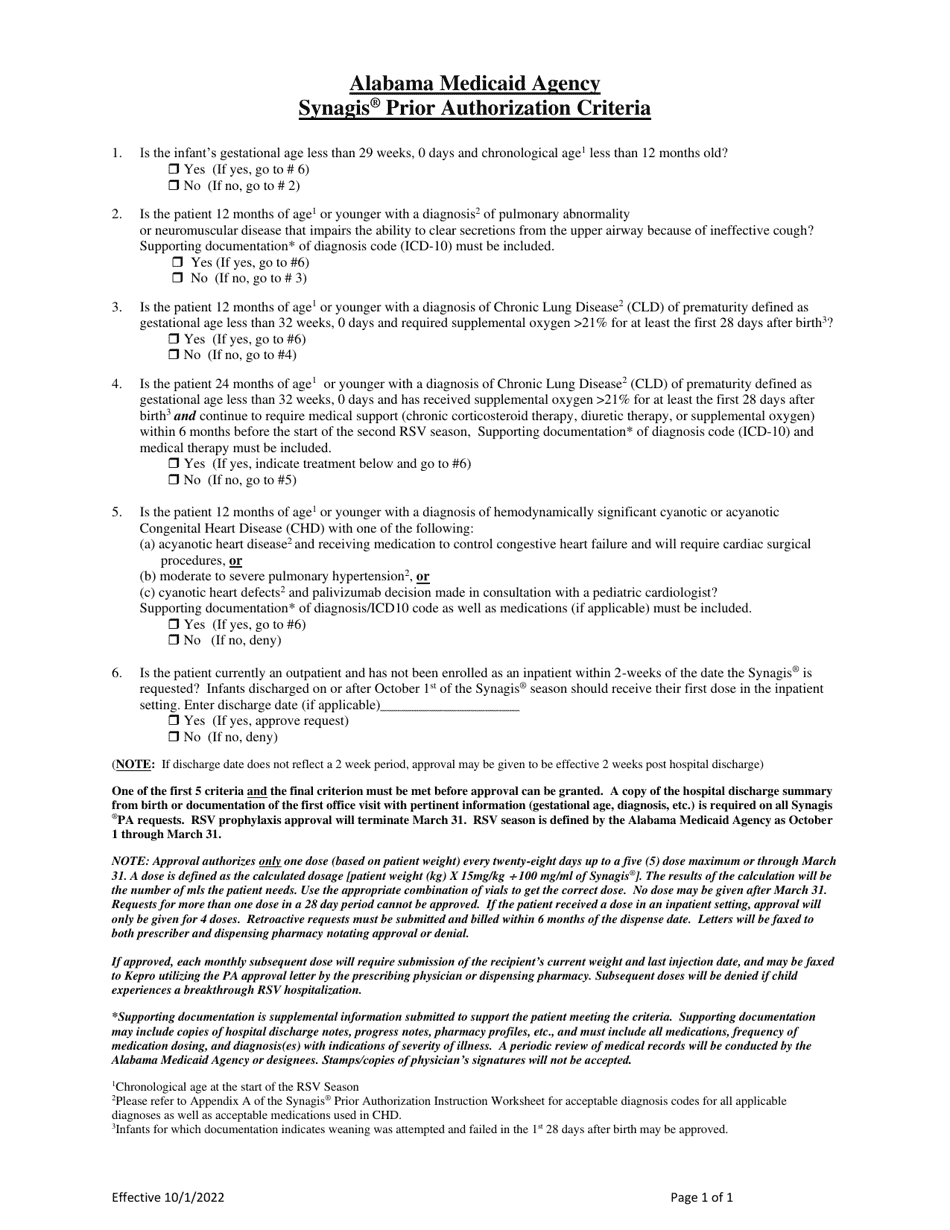
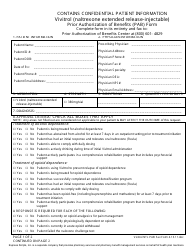
Synagis Prior Authorization Criteria - Alabama
Synagis Prior Authorization Criteria is a legal document that was released by the Alabama Medicaid Agency - a government authority operating within Alabama.
FAQ
Q: What is Synagis?
A: Synagis is a medication used to prevent respiratory syncytial virus (RSV) infection in high-risk infants.
Q: What is respiratory syncytial virus (RSV)?
A: RSV is a common respiratory virus that can cause severe illness, especially in infants and young children.
Q: Who are considered high-risk infants for RSV infection?
A: High-risk infants for RSV infection include premature infants, infants with certain heart or lung conditions, and infants with certain immunodeficiency disorders.
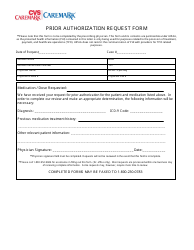
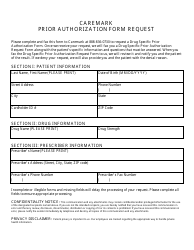
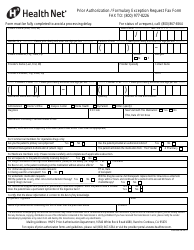
Q: What is prior authorization?
A: Prior authorization is the process of obtaining approval from an insurance company before a medication or treatment is covered.
Q: Why is prior authorization required for Synagis?
A: Prior authorization is typically required for Synagis due to its high cost and specific criteria for use in high-risk infants.
Q: What are the prior authorization criteria for Synagis in Alabama?
A: The specific prior authorization criteria for Synagis in Alabama can vary, but generally, it requires documentation of the infant's high-risk status and a prescription from a healthcare provider.
Q: How can I obtain prior authorization for Synagis?
A: To obtain prior authorization for Synagis, you will need to work with your healthcare provider and insurance company. They will guide you through the process and provide the necessary forms and documentation.
Q: Is prior authorization only required in Alabama?
A: No, prior authorization for Synagis is typically required by insurance companies across the United States, not just in Alabama.
Q: Can prior authorization be obtained retroactively?
A: In most cases, prior authorization cannot be obtained retroactively, meaning it must be obtained before the medication or treatment is administered for coverage to be approved.
Q: What happens if prior authorization is not obtained for Synagis?
A: If prior authorization is not obtained for Synagis, the medication may not be covered by your insurance company, and you may be responsible for paying the full cost out of pocket.
Form Details:
- Released on October 1, 2022;
- The latest edition currently provided by the Alabama Medicaid Agency;
- Ready to use and print;
- Easy to customize;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a printable version of the form by clicking the link below or browse more documents and templates provided by the Alabama Medicaid Agency.