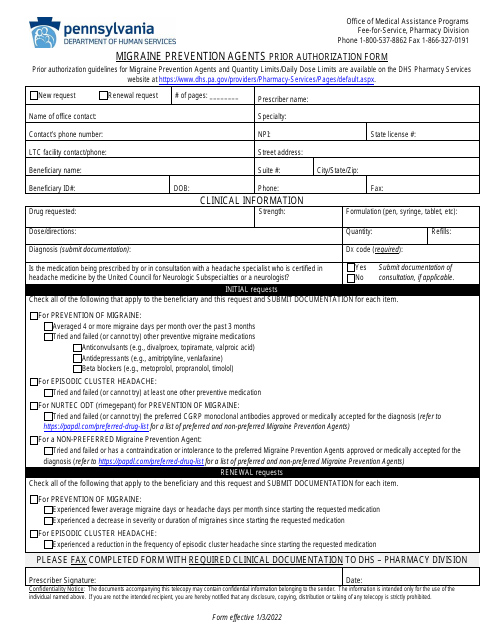
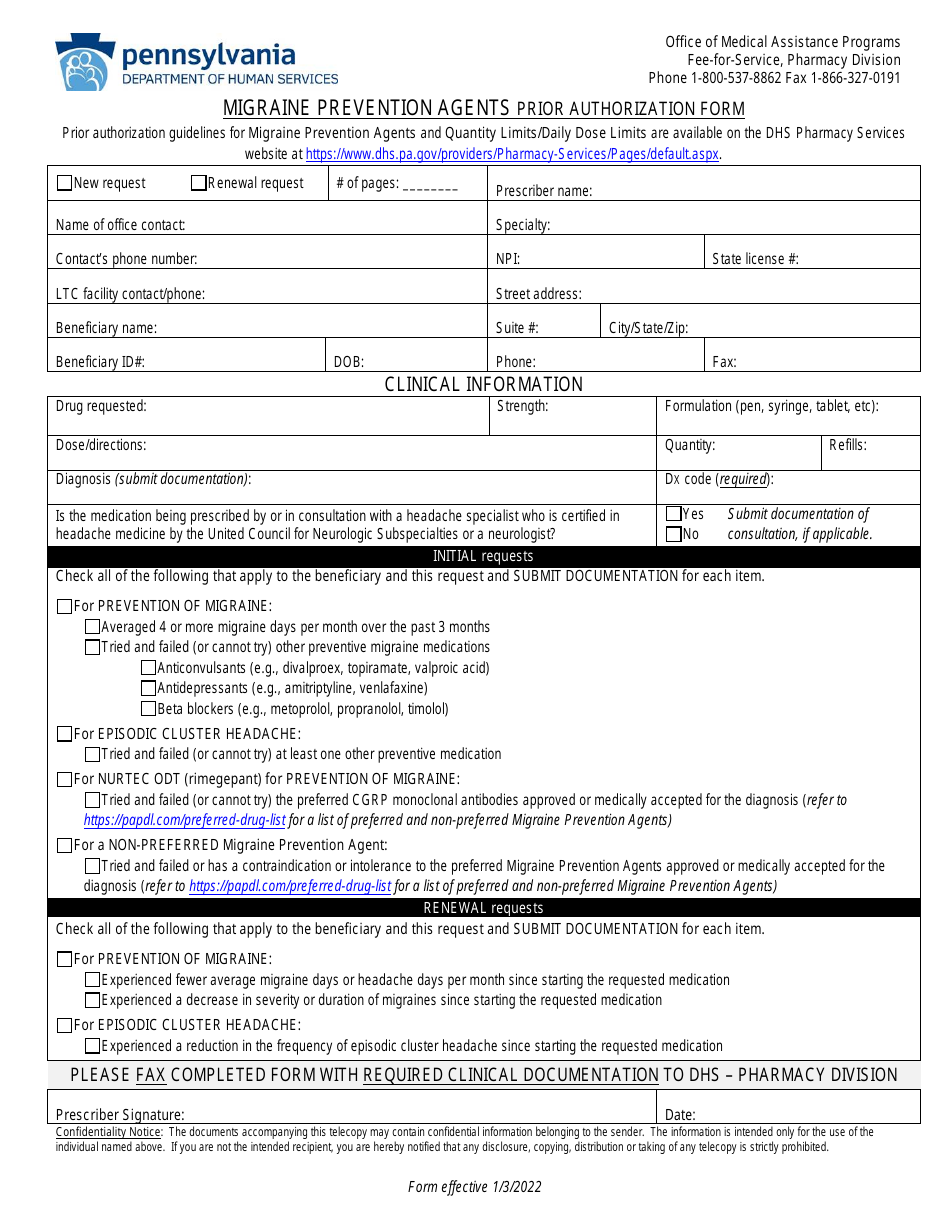
Migraine Prevention Agents Prior Authorization Form - Pennsylvania
The Migraine Prevention Agents Prior Authorization Form - Pennsylvania is a document used by healthcare providers in the state of Pennsylvania to request coverage for a specific medication designed to prevent migraines for their patients. The form needs to be submitted to the patient's insurance company for review. This process is called prior authorization. It basically means that before the insurance company agrees to cover the cost of this particular medication, they need to approve it first, based on the information provided in this form. This process is oftentimes used for medications that are costly or could have potential for misuse or harm.
The Migraine Prevention Agents Prior Authorization Form in Pennsylvania is typically filed by a healthcare provider or a physician. They fill out the form to request coverage for a specific migraine prevention medication for their patient under the patient's health insurance plan. The filled form is then sent to the insurance company for approval.
FAQ
Q: What is a Migraine Prevention Agents Prior Authorization Form in Pennsylvania?
A: The Migraine Prevention Agents Prior Authorization Form is a form used by medical professionals in Pennsylvania, USA to request coverage for specific migraine prevention medications. It helps to verify that prescribed medications are covered under a patient’s health plan.
Q: Who uses the Migraine Prevention Agents Prior Authorization Form in Pennsylvania?
A: The Migraine Prevention Agents Prior Authorization Form in Pennsylvania is used by healthcare providers. Providers fill out this form when they prescribe migraine prevention medications that require prior authorization from the patient’s insurance company.
Q: Why is the Migraine Prevention Agents Prior Authorization Form necessary?
A: The form is necessary to get approval from an insurance company before certain medications are covered under the patient’s health plan. If medication is prescribed that is not normally covered, or is outside the regular coverage rules, then a prior authorization request needs to be made.
Q: How to submit the Migraine Prevention Agents Prior Authorization Form in Pennsylvania?
A: Once a healthcare provider fills out the form, it is typically sent to the patient's insurance company. The process for this can vary, but may involve faxing, mailing, or electronically submitting the form. It's essential to follow the insurance company's specific submission guidelines.
Q: What happens after submitting the Migraine Prevention Agents Prior Authorization Form in Pennsylvania?
A: Once the form is submitted to the insurance company, they review the request. The approval or denial for coverage is then communicated back to the healthcare provider, and then usually relayed to the patient. The time for this process can vary.