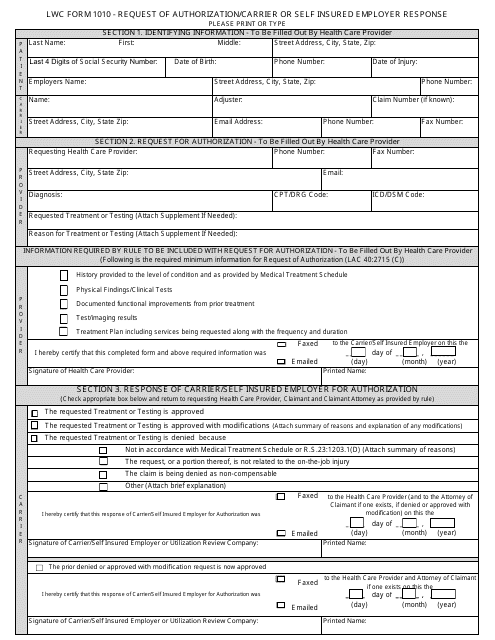
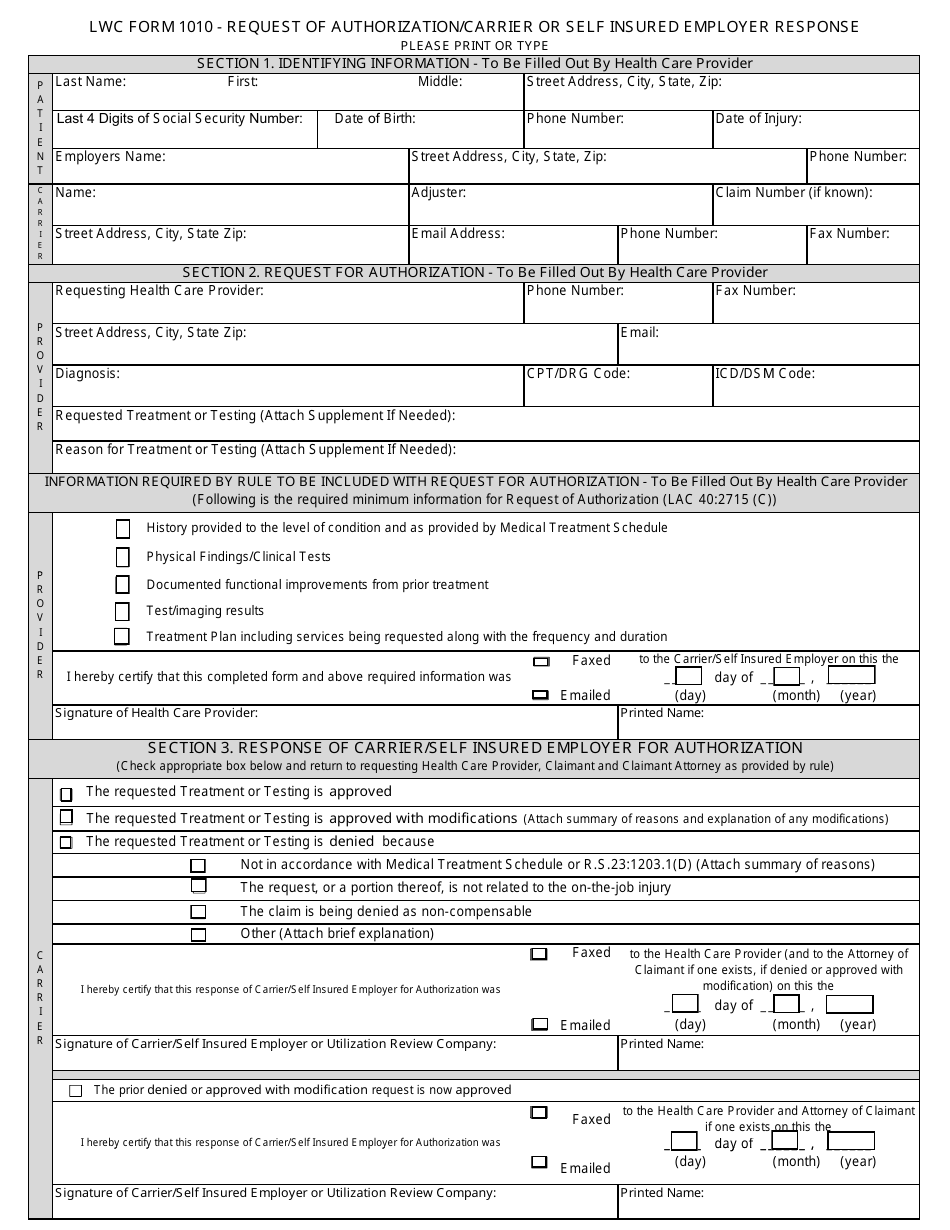
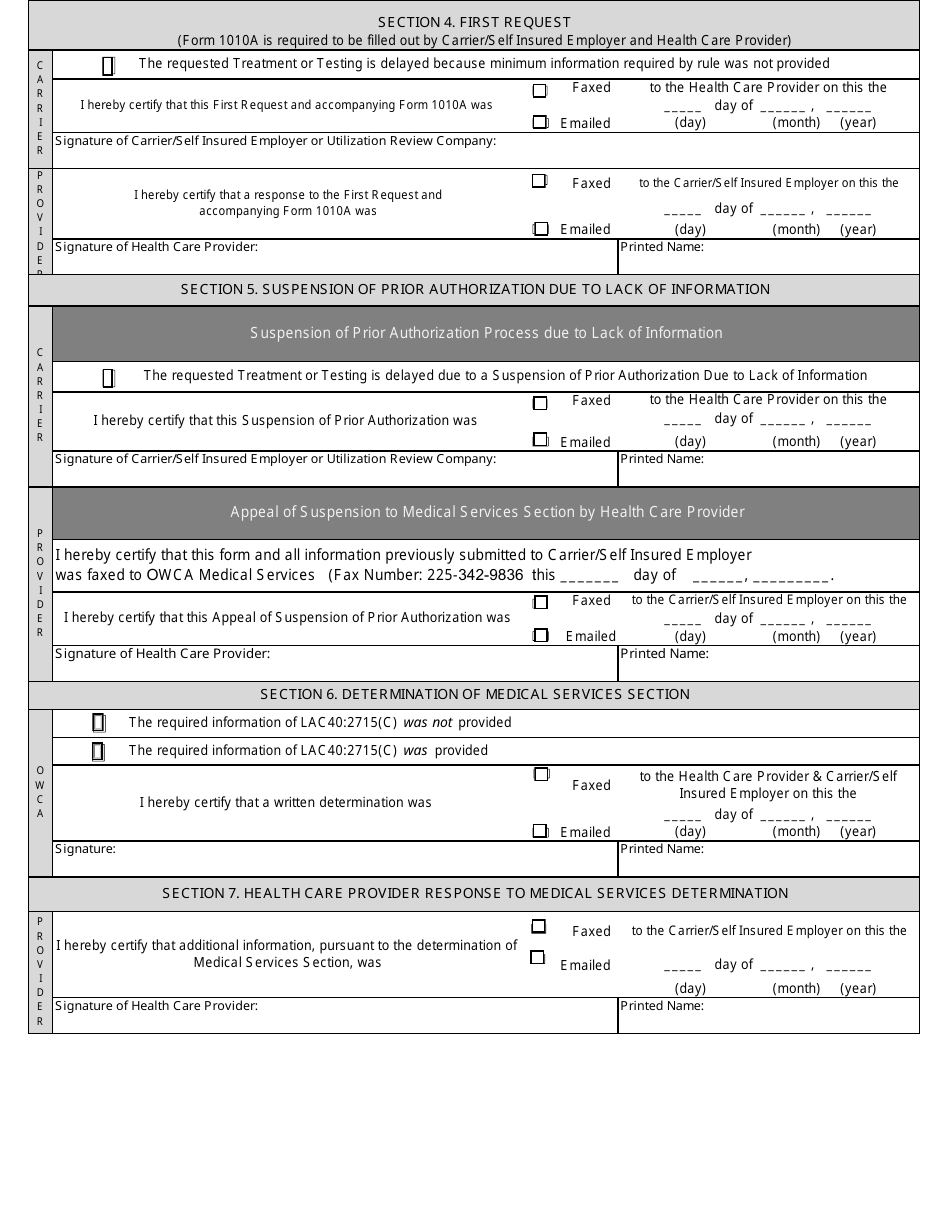
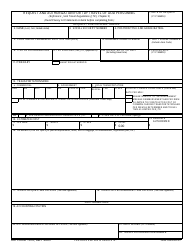
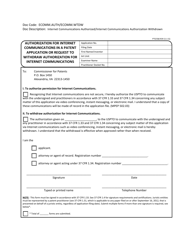
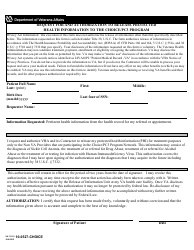
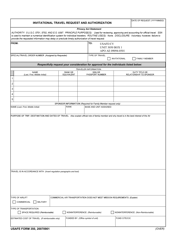
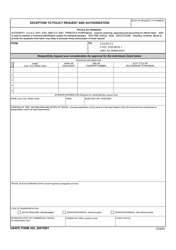
Form 1010 Request of Authorization / Carrier or Self Insured Employer Response
What Is Form 1010?
This is a legal form that was released by the U.S. Department of Labor and used country-wide. As of today, no separate filing guidelines for the form are provided by the issuing department.
FAQ
Q: What is Form 1010?
A: Form 1010 is a document used to request authorization from a carrier or self-insured employer.
Q: Who uses Form 1010?
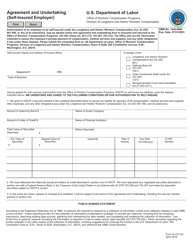
A: Form 1010 is used by individuals or organizations seeking authorization from a carrier or self-insured employer.
Q: What is the purpose of Form 1010?
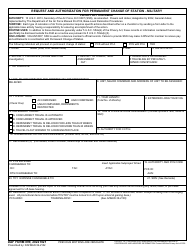
A: The purpose of Form 1010 is to obtain authorization to provide services or treatment to individuals under the workers' compensation system.
Q: How do I obtain Form 1010?
A: Form 1010 can be obtained from the appropriate workers' compensation board or insurance carrier.
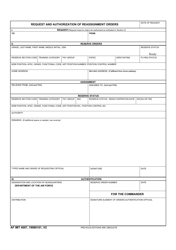
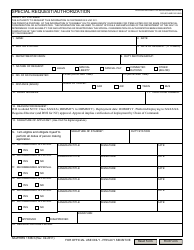
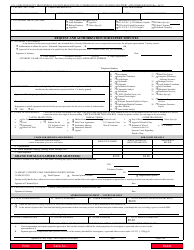
Q: What information is required on Form 1010?
A: Form 1010 typically requires information such as the name and contact information of the individual or organization requesting authorization, details of the proposed services or treatment, and any supporting documentation.
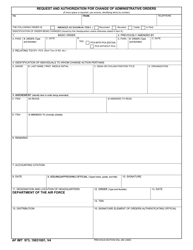
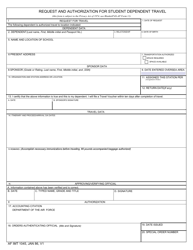
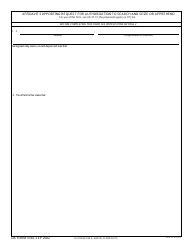
Q: What happens after submitting Form 1010?
A: After submitting Form 1010, the carrier or self-insured employer will review the request and make a decision on whether to authorize the requested services or treatment.
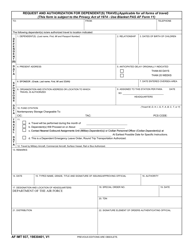
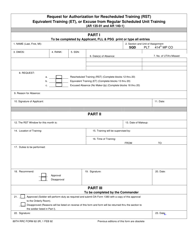
Form Details:
- The latest available edition released by the U.S. Department of Labor;
- Easy to use and ready to print;
- Yours to fill out and keep for your records;
- Compatible with most PDF-viewing applications;
- Fill out the form in our online filing application.
Download a fillable version of Form 1010 by clicking the link below or browse more documents and templates provided by the U.S. Department of Labor.