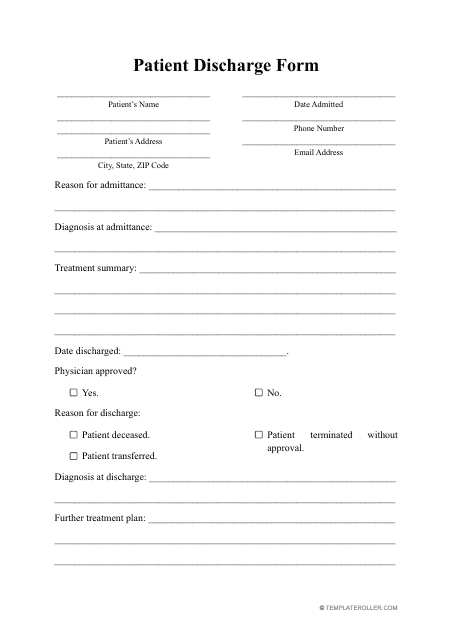
Patient Discharge Form
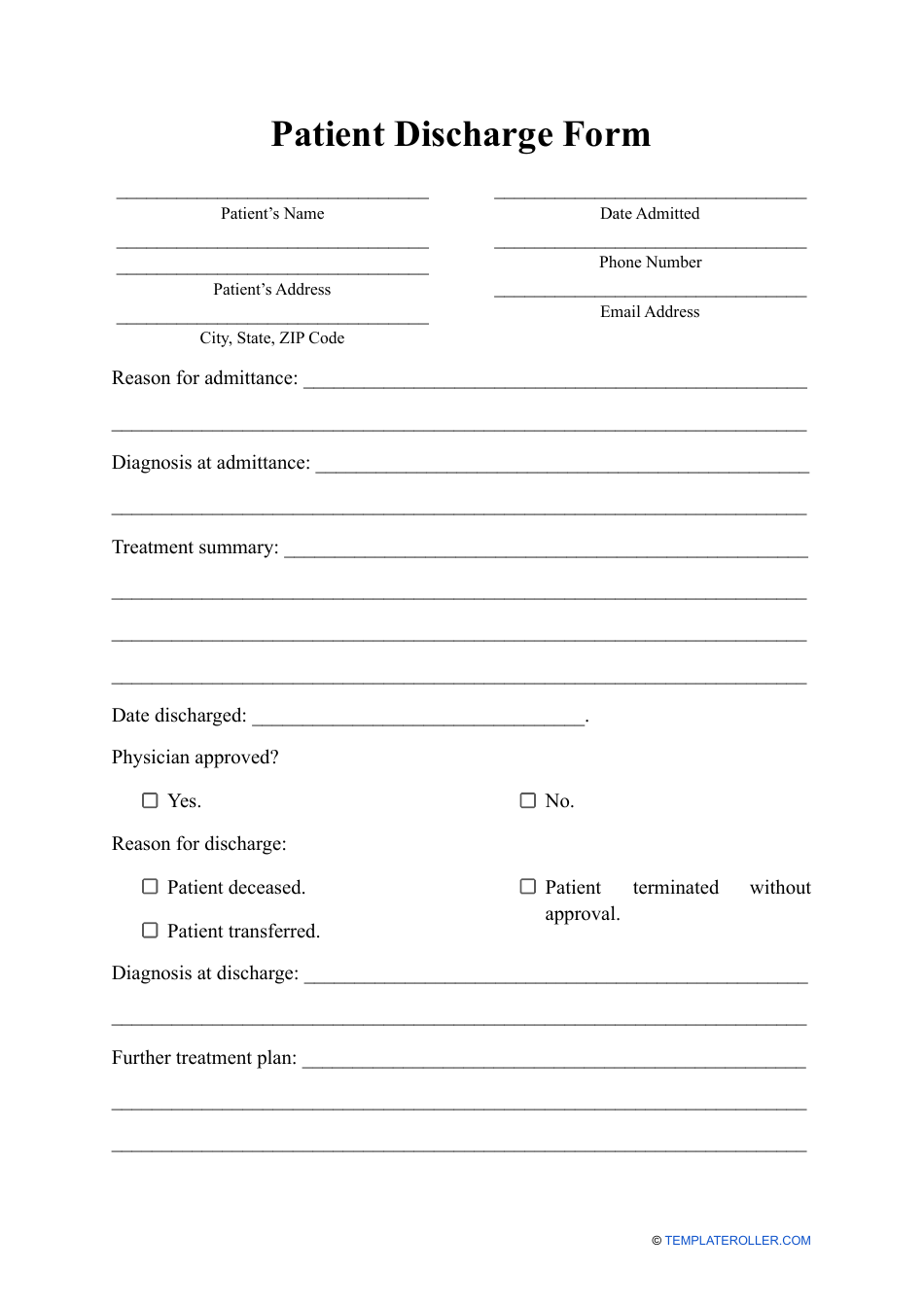
A Patient Discharge Form is used to document the release of a patient from a healthcare facility, such as a hospital or clinic. It includes information about the patient's condition, treatment received, medications prescribed, and instructions for ongoing care. The form is important for coordinating care between healthcare providers and ensuring a smooth transition for the patient after their hospital stay.
The patient discharge form is typically filed by the healthcare facility or hospital where the patient was receiving treatment.
FAQ
Q: What is a patient discharge form?
A: A patient discharge form is a document that is filled out when a patient is ready to leave a healthcare facility.
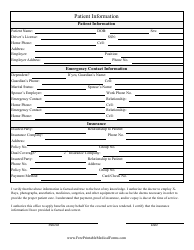
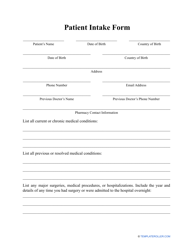
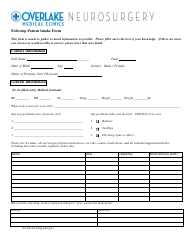
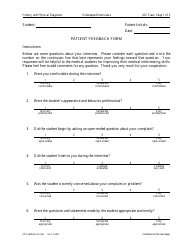
Q: What information is included in a patient discharge form?
A: A patient discharge form typically includes the patient's name, date of discharge, reason for discharge, post-discharge instructions, and any necessary follow-up appointments or referrals.
Q: Why is a patient discharge form important?
A: A patient discharge form is important because it ensures that all necessary information is communicated to the patient and their follow-up care providers, helping to ensure a smooth transition and continuity of care.
Q: Who fills out a patient discharge form?
A: A patient discharge form is usually filled out by a healthcare professional, such as a doctor or nurse, who is responsible for the patient's care during their stay at the healthcare facility.
Q: What should a patient do with a completed discharge form?
A: A patient should keep a copy of their completed discharge form for their own records and provide a copy to their primary care physician or any other healthcare providers involved in their post-discharge care.