Free Hospital Forms and Templates
If your medical facility is looking for new methods and strategies to optimize the efficiency of services you provide, improve internal operations, and upgrade communication between various departments and employees, it is advised to give serious consideration to proper recordkeeping - keep track of all the patients that visit your clinic, remember their decisions regarding their health, and facilitate interactions with insurance providers. Learn more about Hospital Forms , maintain comprehensive records in your institution, and ensure your patients get the care they deserve.
For a full list of Hospital Form templates please check out our library below.
Hospital Form Types
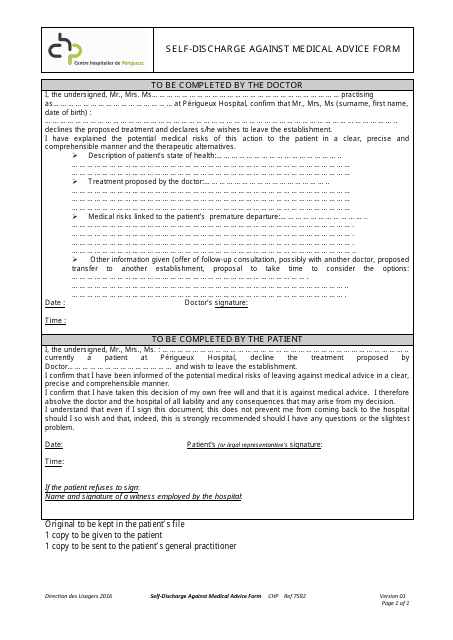
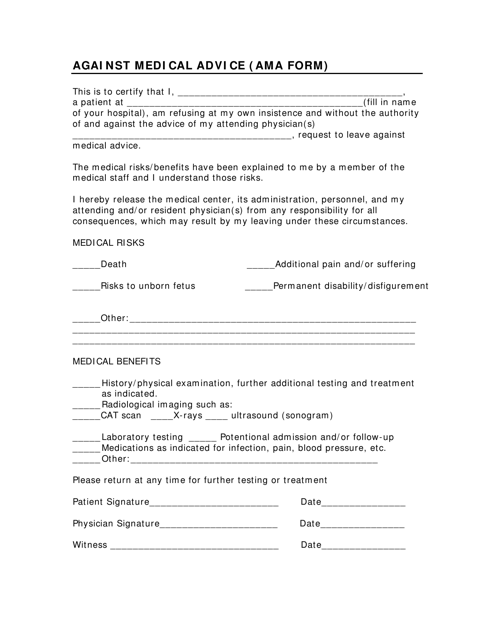
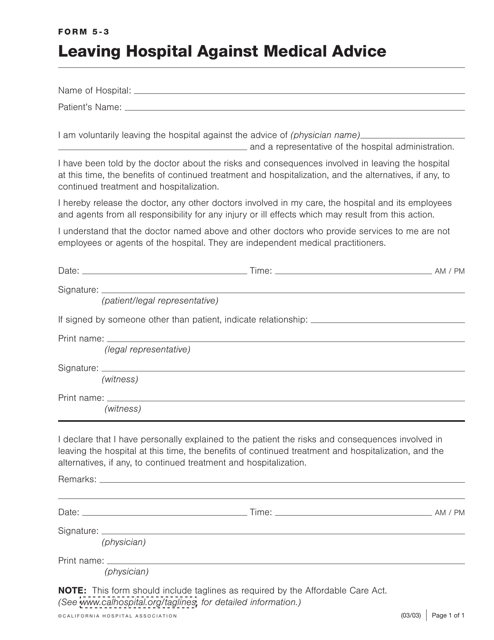
- AMA Form. In case a patient chooses to leave the hospital despite recommendations of the doctor treating them, they are within their rights to do so, and your obligation is to give them an AMA Form to confirm they refuse to complete the treatment or undergo a scheduled procedure. This document will prove doctors and nurses are released from any liability for potential negative consequences the decision of the patient may have and it can be signed for any personal reason the individual in question shares or does not share;
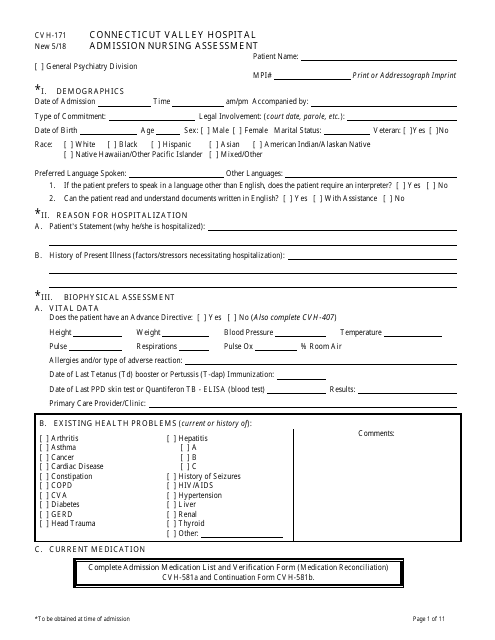
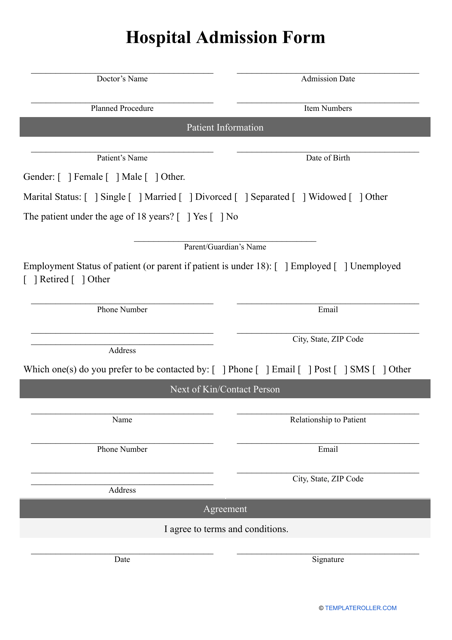
- Hospital Admission Form. A patient can be admitted to a medical institution because it was planned by them and their doctor or arrive at the hospital with a serious injury or being severely ill - the administrator of the facility has to ask them (if that is possible) to fill out a Hospital Form that lists their personal information and symptoms they experience. Alternatively, the paperwork is completed by a medical professional or a person representing the patient in case they are unable to communicate their sensations;
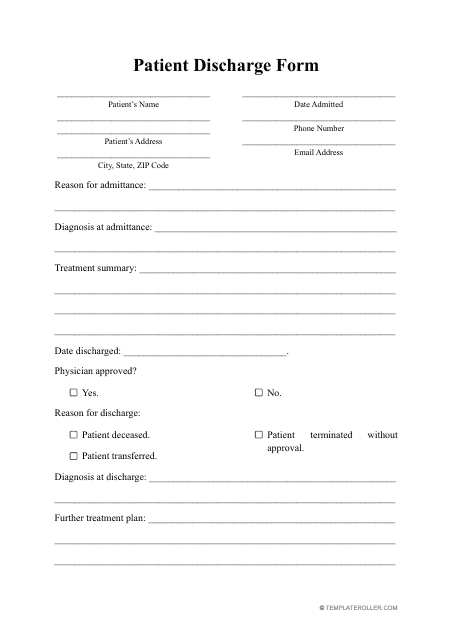
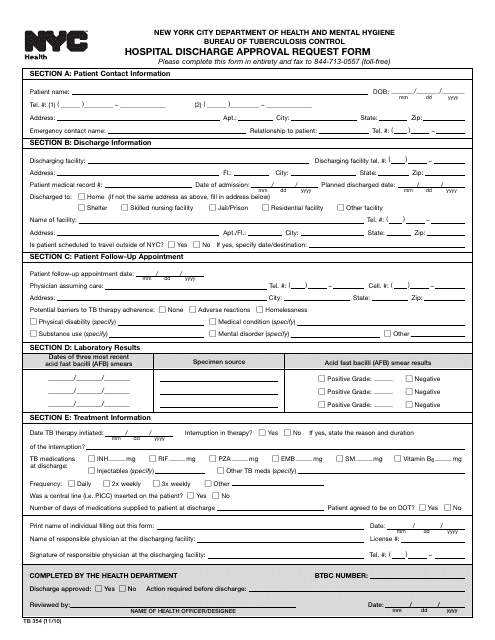
- Hospital Discharge Form. Once the patient is ready to leave the hospital, there should be a formal record of this event - use this instrument to verify their departure is supported by their physician, elaborate on the treatment they have received so far, and specify whether the patient is supposed to follow any recommendations or take prescribed medication when they are no longer under constant medical supervision;
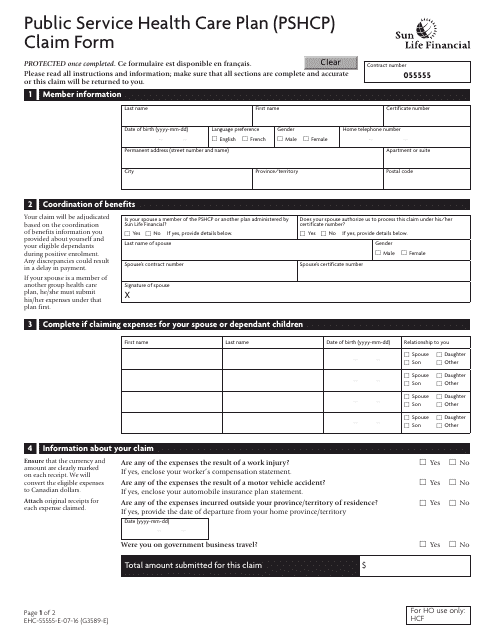
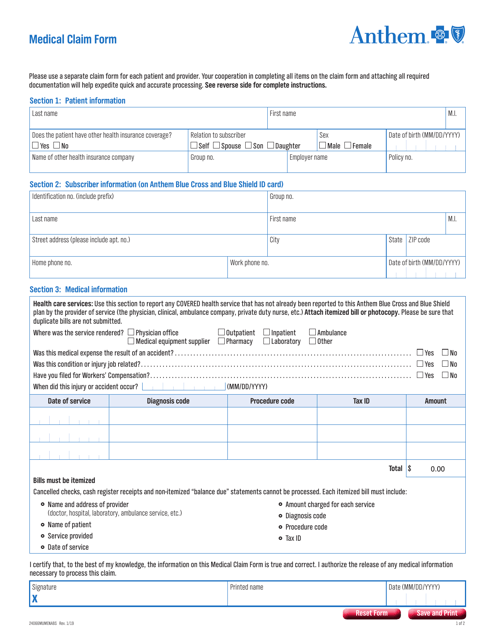
- Medical Claim Form. Fill out this statement to let the insurance company know about the diagnosis of the patient and proposed treatment including medication, equipment, and transportation they may require - this way, the ill or injured individual will have an opportunity to receive compensation for the medical bills issued in their name.
Haven't found the form you're looking for? Take a look at the related templates below:
Documents:
13
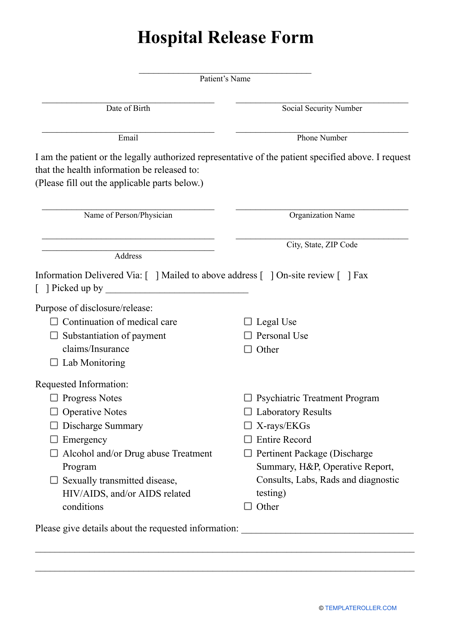
This form is used for documenting the release of a patient from a hospital or healthcare facility. It includes important information about the patient's condition, treatment received, and any follow-up instructions.
This type of document is used when a patient chooses to leave the hospital against the advice of medical professionals.
This document is for submitting claims to the Public Service Health Care Plan (PSHCP), which is a health insurance program for public service employees in Canada. The form is administered by Sun Life Financial.
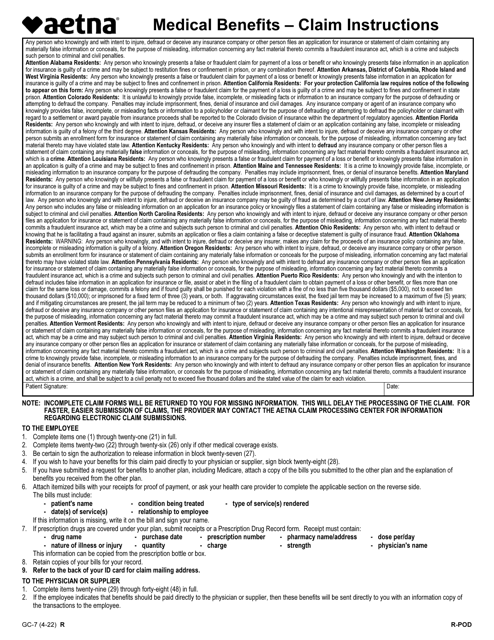
This form is a formal instrument used to ask Aetna - a healthcare insurance company - for reimbursement after a patient has paid for medical services out of their own pocket.
This form is used for submitting medical claims to Anthem insurance company.
This form is used for documenting when a patient decides to leave the hospital or medical facility against the advice of their healthcare provider. It helps protect healthcare professionals and the facility by obtaining the patient's acknowledgment of the risks and consequences of leaving against medical advice.
This document provides information on leaving the hospital against medical advice as it pertains to the California Hospital Association in California.
This document is utilized for the intake process at Connecticut Valley Hospital, allowing medical professionals to assess a new patient's nursing needs upon admission. It encompasses a wide range of health factors crucial to designing an effective care plan.
This Form is used for hospital admissions. It collects important information about the patient, such as personal details, medical history, and reason for admission. It is necessary for efficient and accurate patient care.
This form is used for patients to be released from the hospital after receiving medical treatment. It includes important information about the patient's condition, treatment received, and follow-up care instructions.
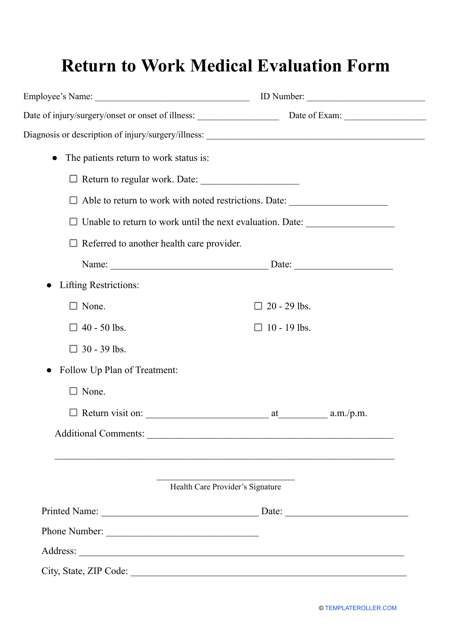
This form is used for providing the necessary documentation from a doctor to confirm that an individual is medically fit to return to work after a period of absence.
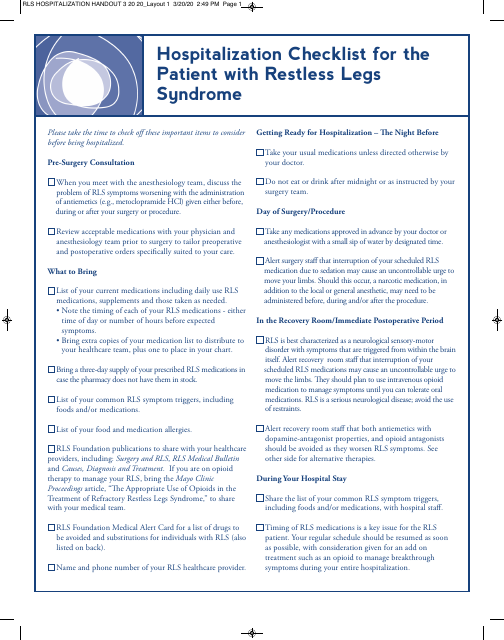
This document provides a comprehensive checklist for individuals with Restless Legs Syndrome (RLS), assisting in their hospital stay. It provides guidance on medications, treatments, and accommodations to ensure optimum comfort and care for RLS patients.
This form is used by healthcare providers in New York City to request approval for discharging a patient from the hospital. It's an essential component for patient transition towards outpatient care or other post-hospital medical facilities.