Free Hospital Discharge Forms and Templates
Hospital Discharge Form: What Is It?
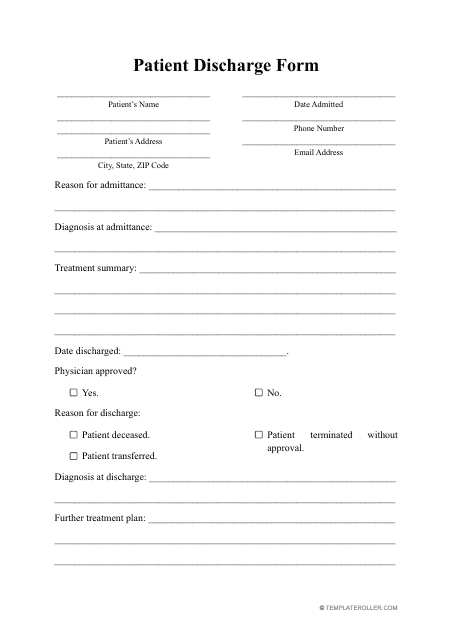
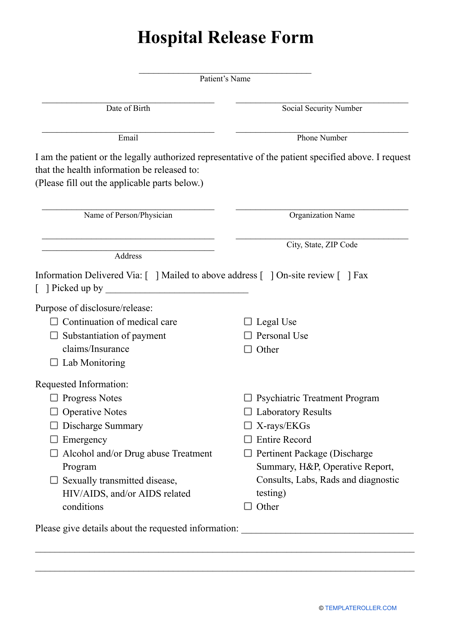
A Hospital Discharge Form refers to a document which is given to patients who have been discharged from a hospital after receiving medical treatment or care.
Alternate Names:
- Patient Discharge Form;
- Hospital Discharge Papers;
- Medical Hospital Discharge Papers;
- Hospital Release Form.
The form contains important information about:
- The patient’s health status;
- Their treatment plan;
- Instructions for post-hospital care.
It serves as a communication tool between the hospital and the patient’s primary care provider, ensuring continuity of care. The form typically includes the patient’s personal information such as:
- Their name and address;
- Their date of birth;
- Recent contact information including phone number and email;
- It also includes details about the patient’s medical history, diagnosis, and treatment plan. This information is critical for the patient’s primary care provider to understand the patient’s health status and to provide appropriate follow-up care.
A standard Hospital Release Form will also provide instructions for the patient’s post-hospital care. This may include information about medications, wound care, physical therapy, and follow-up appointments. The instructions are tailored to the patient’s specific needs and are designed to help the patient recover and avoid complications.
In addition to instructions for post-hospital care, the discharge form may also include information about the patient’s rights and responsibilities. This may include information about privacy laws, patient advocacy, and complaint procedures.
For a full list of Hospital Discharge Form templates please feel free to check out our library below.
How Long Does Hospital Discharge Take?
Hospital Discharge is the process by which a patient is released from the hospital after receiving medical treatment. The length of time it takes for a hospital discharge to be completed can vary depending on several factors:
- The first factor that can affect the length of a hospital discharge is the complexity of the patient's medical condition . Patients who have undergone major surgery or who have serious medical conditions may require more time to be discharged. In these cases, the medical team may need to perform additional tests and evaluations to ensure that the patient is stable enough to leave the hospital;
- Another factor that can impact the length of a hospital discharge is the availability of follow-up care . Patients who require ongoing medical treatment, such as physical therapy or home health care, may need to wait for these services to be arranged before they can be discharged. This can add several days or even weeks to the discharge process;
- The hospital's administrative processes can also contribute to the length of a hospital discharge . Patients may need to complete paperwork, receive discharge instructions, and make arrangements for transportation or medication before they can leave the hospital. These tasks can take several hours or even days to complete;
- Finally, the patient's own preferences and needs can affect the length of a hospital discharge . Some patients may prefer to stay in the hospital longer to receive additional care or support, while others may be eager to return home as soon as possible.
Still looking for a particular form? Take a look at the related templates and forms below:
Documents:
8
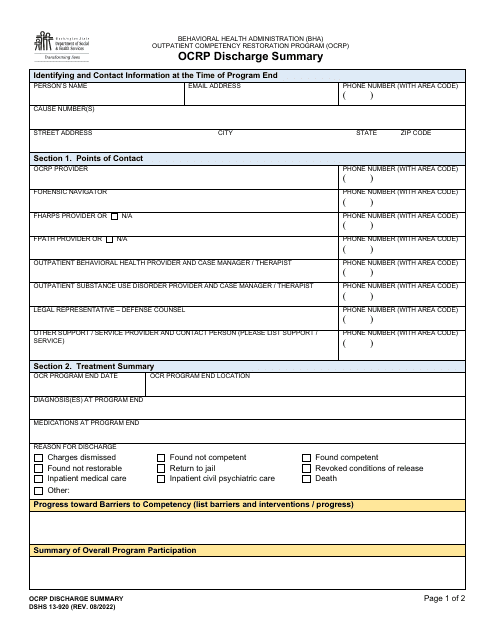
This form is used for documenting the release of a patient from a hospital or healthcare facility. It includes important information about the patient's condition, treatment received, and any follow-up instructions.
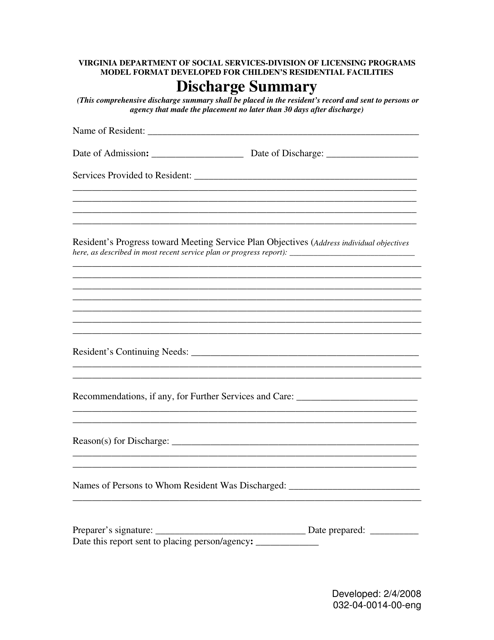
This document is used for creating a summary of a patient's discharge from a healthcare facility in Virginia.
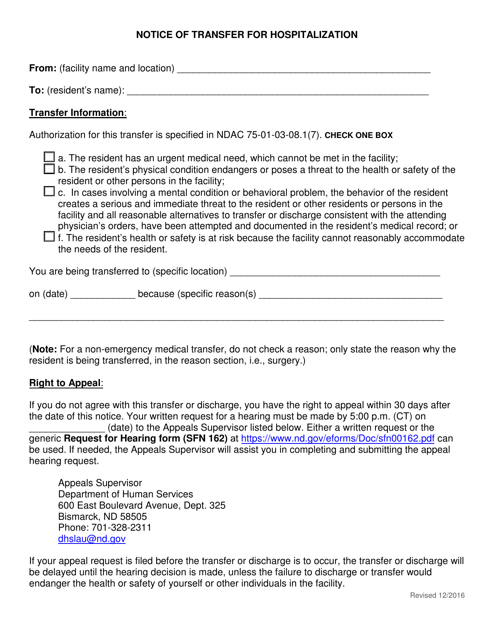
This form is used for notifying the transfer of a patient to another hospital for hospitalization in the state of North Dakota.
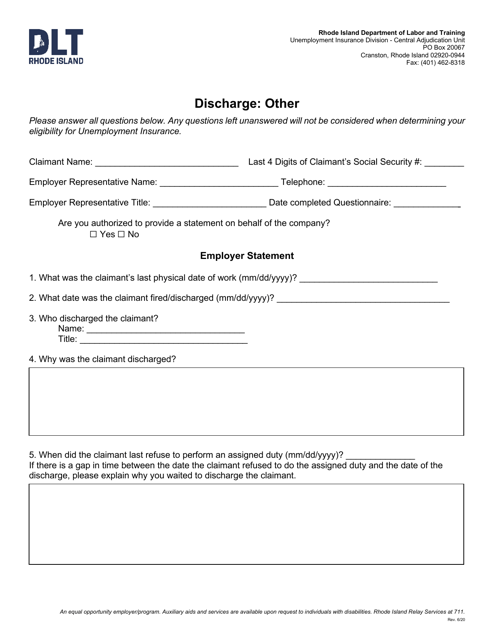
This type of document is used for the discharge of a mortgage or lien in the state of Rhode Island.
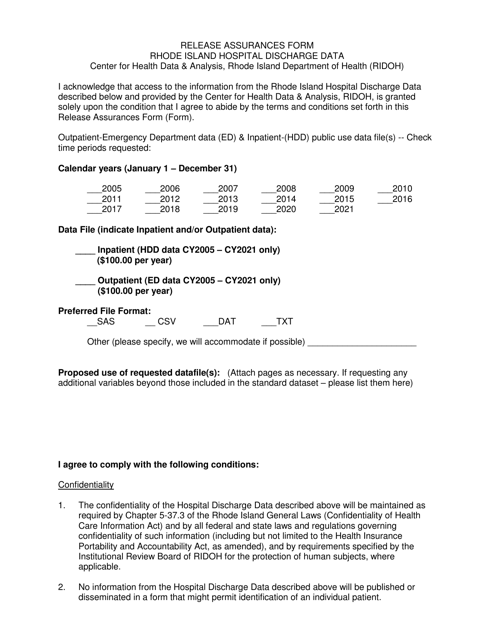
This form is used for ensuring the proper release and protection of Rhode Island hospital discharge data.
This form is used for patients to be released from the hospital after receiving medical treatment. It includes important information about the patient's condition, treatment received, and follow-up care instructions.
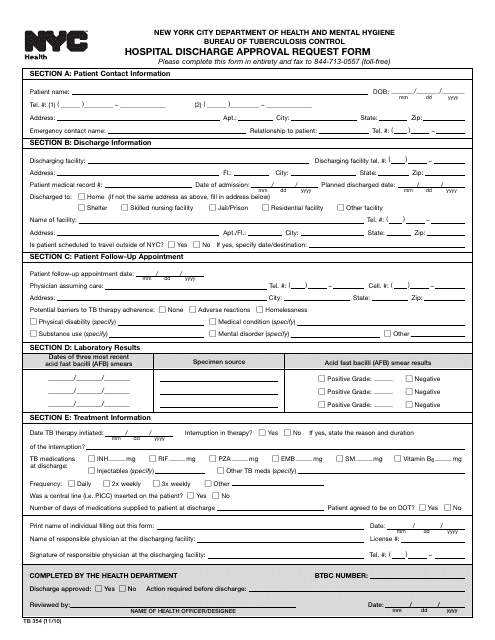
This form is used by healthcare providers in New York City to request approval for discharging a patient from the hospital. It's an essential component for patient transition towards outpatient care or other post-hospital medical facilities.