Mental Health Templates
Documents:
727
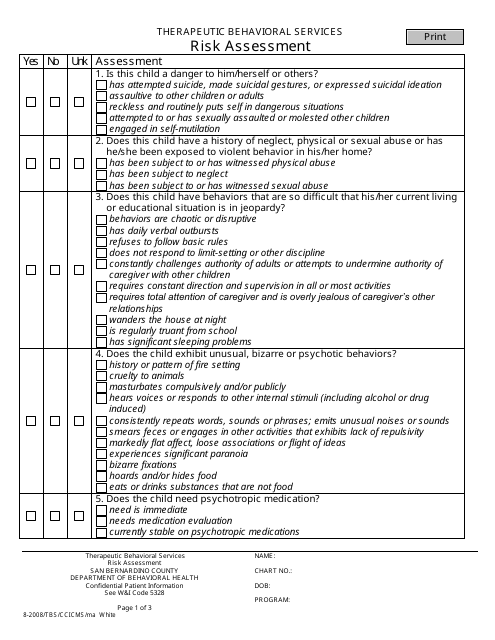
This document is a risk assessment form specifically designed for Therapeutic Behavioral Services in San Bernardino County, California. It helps identify potential risks and develop strategies to mitigate them.
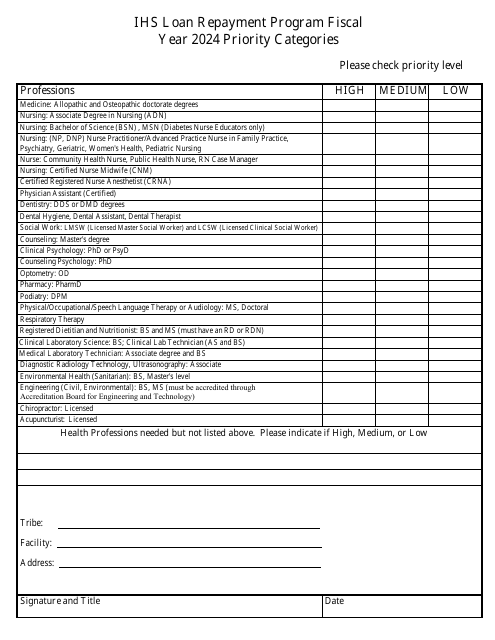
This document provides information about the priority categories for the IHS Loan Repayment Program. The program helps healthcare professionals in certain priority areas repay their loans.
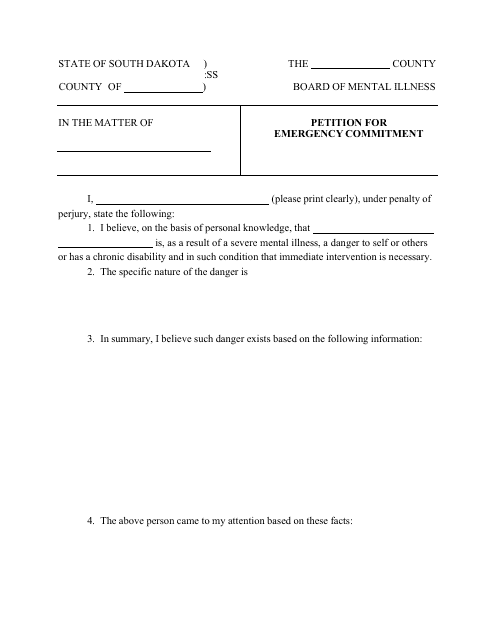
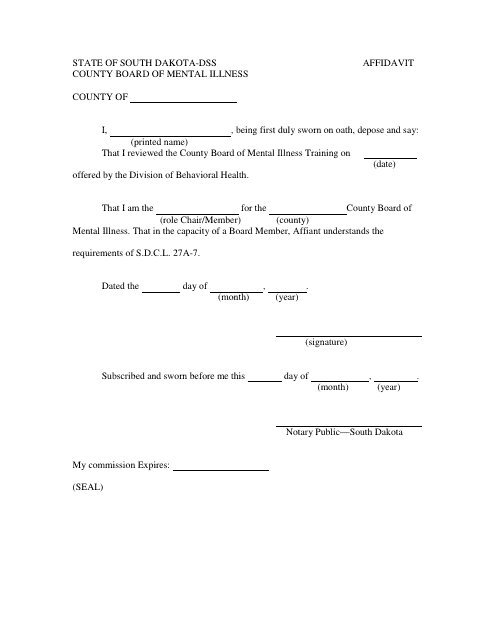
This type of document is used in South Dakota for filing a petition to request emergency commitment of an individual.
This document is used for providing a written statement under oath in the County Board of Mental Illness in South Dakota. It is used to declare facts and information related to mental illness cases.
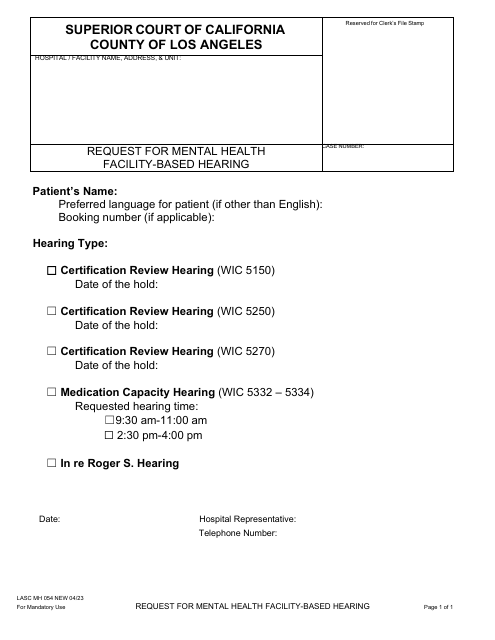
Form LASC MH054 Request for Mental Health Facility-Based Hearing - County of Los Angeles, California
This form is used by individuals residing in Los Angeles County, California, who wish to request a hearing concerning their situation and treatment at a mental health facility. It helps to ensure that individuals receive fair and appropriate treatment by ensuring their concerns are heard by county officials.
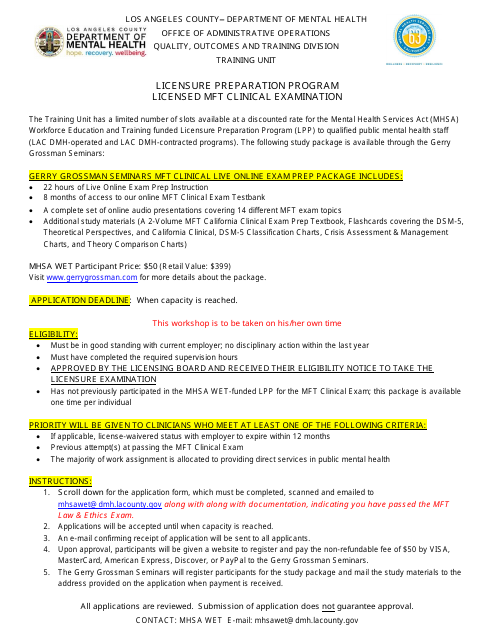
This document provides guidelines and information about the Marriage and Family Therapist Clinical Examination, a necessary step for licensure in Los Angeles County, California. It includes instructions about the application process, examination details, and other relevant information for hopeful MFTs.
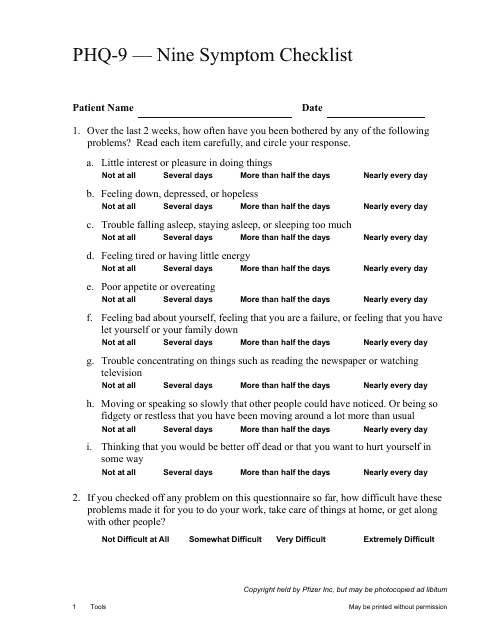
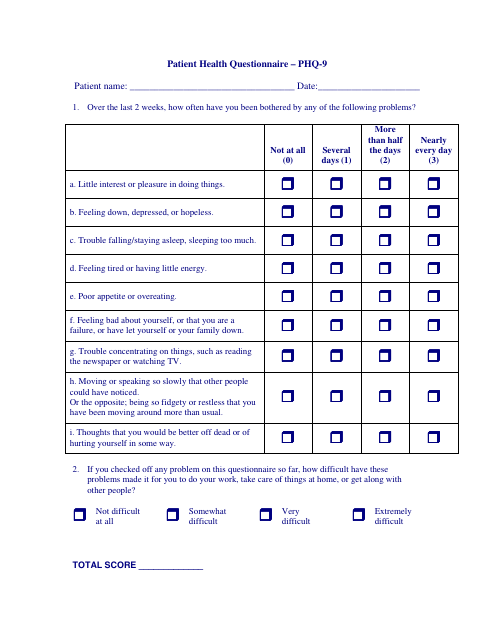
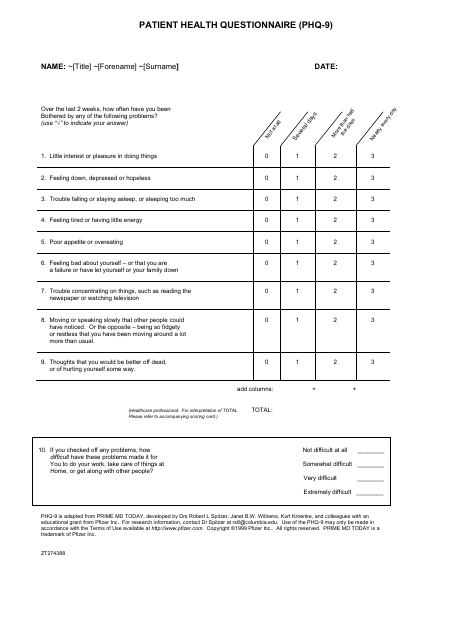
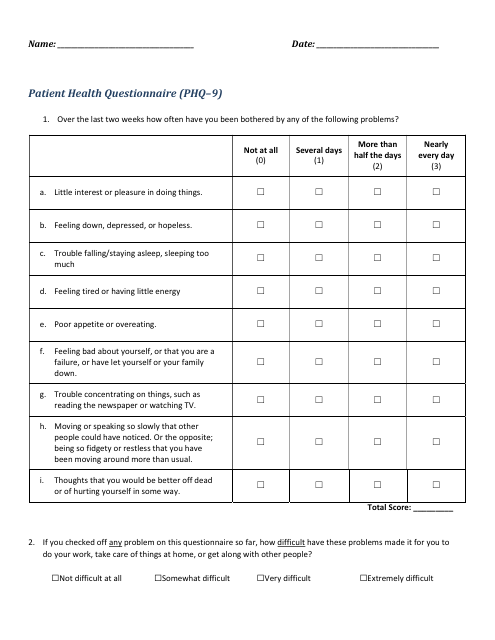
This type of document is a nine-item checklist that is used to assess the severity of depressive symptoms. It is often used by healthcare professionals to help diagnose and monitor depression.
This type of document is a self-rated measure used by the American Psychiatric Association to assess the symptoms of adults using the DSM-5 framework.
This document provides a measure for assessing the severity of depression in adults, developed by the American Psychiatric Association.
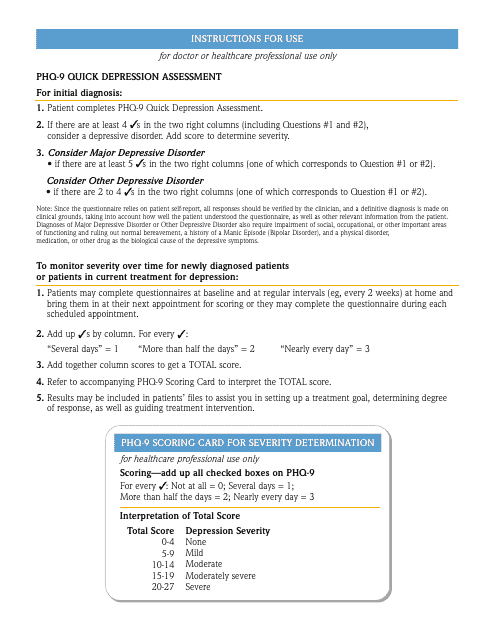
This document provides a quick assessment tool, called PHQ-9, developed by Pfizer, for evaluating depression symptoms.
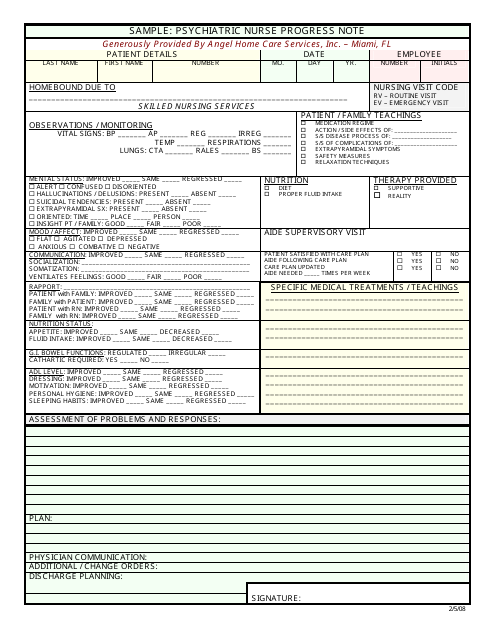
This type of document is used by psychiatric nurses to write down observations and progress made by patients during their treatment sessions.
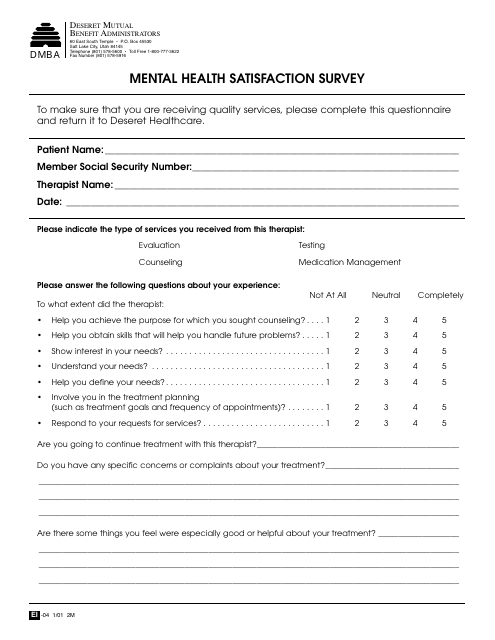
This document is a survey that measures the satisfaction levels of individuals regarding their mental health. It aims to gather feedback on the quality of mental health services and support provided to individuals.
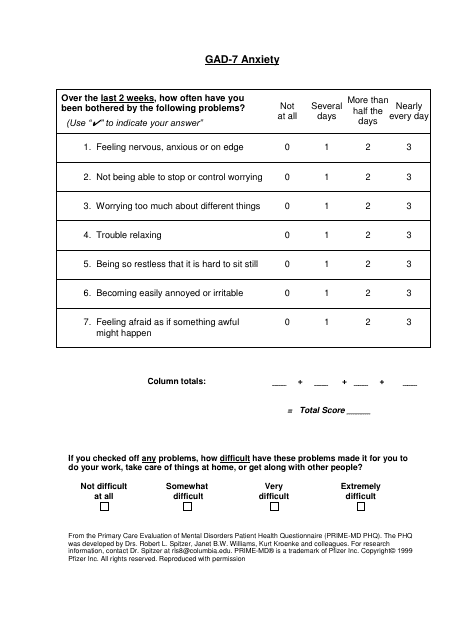
This document is a chart used for assessing anxiety and depression levels using the Gad-7 and Phq-9 scales. It helps in understanding and tracking symptoms of anxiety and depression.
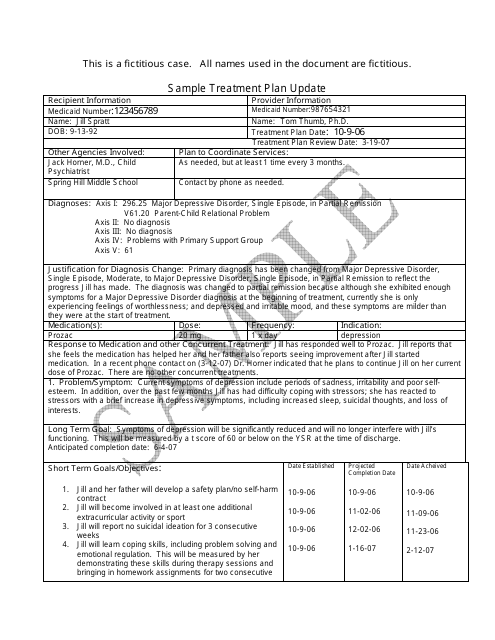
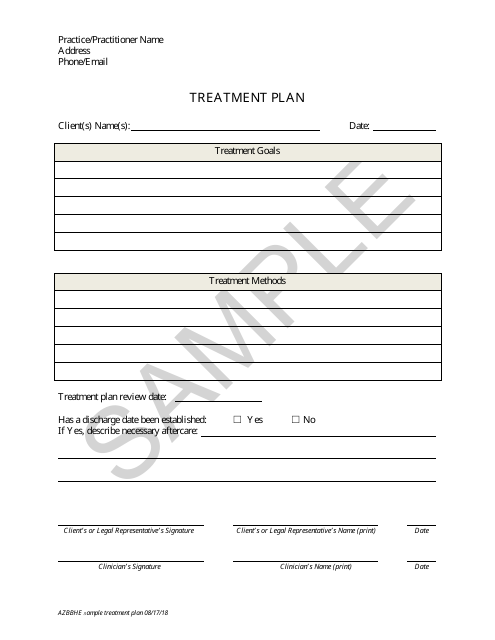
This document provides an updated treatment plan for a patient's medical condition. It outlines any changes or adjustments made to their current course of treatment.
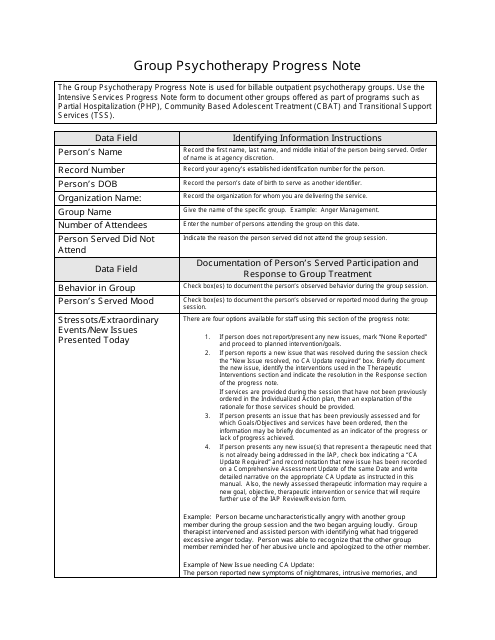
This type of document is used to record the progress of individuals participating in group therapy sessions. It helps track the development and goals achieved throughout the therapy process.
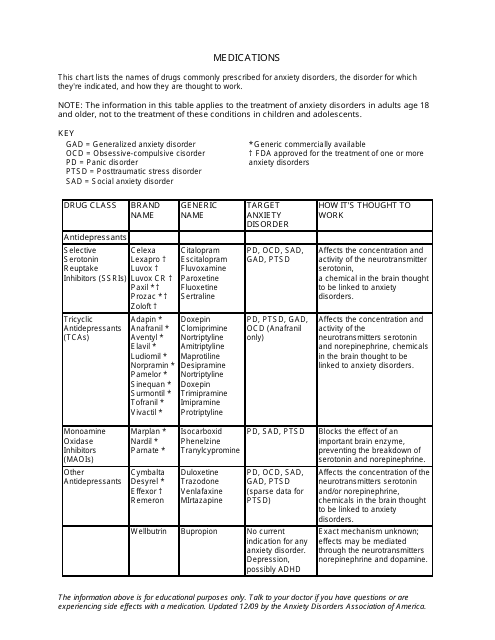
This document provides a chart listing different medications used to treat anxiety disorders. It includes information on the names, dosage, and possible side effects of these medications. The chart can be helpful for individuals seeking information on the various options available for managing anxiety.
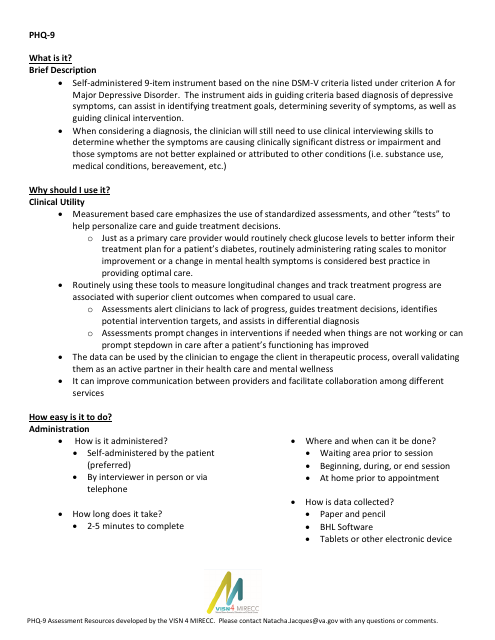
This form is used to assess a patient's mental health using the PHQ-9 questionnaire. It is specifically implemented within the Veterans Integrated Service Network (VISN) 4 Mental Illness Research, Education, and Clinical Center (MIRECC).
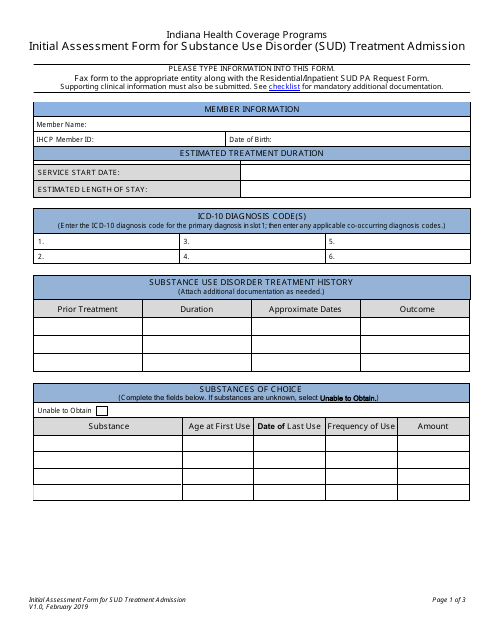
This document is utilized for initial evaluation of individuals seeking admission for Substance Use Disorder Treatment in Indiana health coverage programs. It is beneficial for understanding the patient's condition and treatment needs.
This document is a mental health assessment tool used to evaluate a person's mental well-being and identify potential mental health concerns. It helps healthcare professionals assess and diagnose mental disorders and provide appropriate treatment.
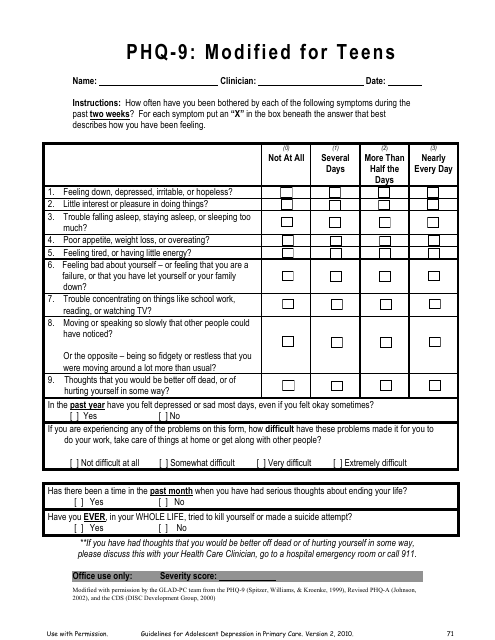
This Form is used for assessing depression symptoms in teenagers using a modified version of the PHQ-9 questionnaire.
This document is designed for evaluating a patient's mental health status. It's widely used by healthcare professionals to screen for depression and monitor treatment progress.
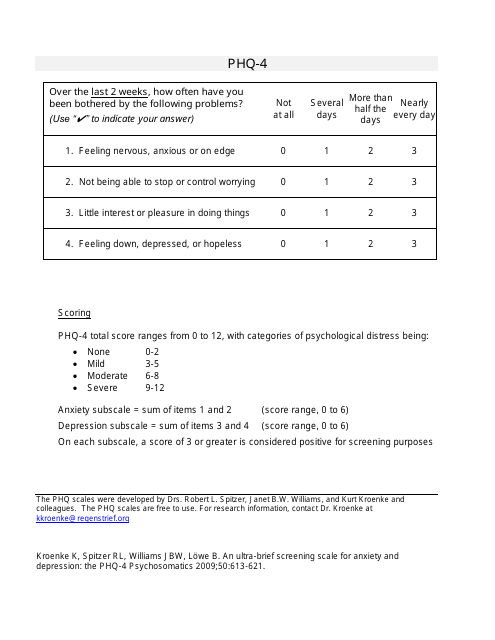
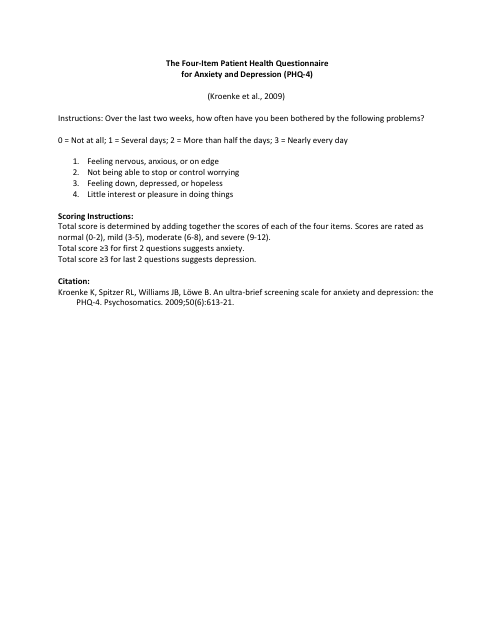
This document is a questionnaire known as the PHQ-4 scale. It is used to assess an individual's level of anxiety and depression.
This form is used for assessing anxiety and depression in patients. The Four-Item Patient Health Questionnaire for Anxiety and Depression (PHQ-4) consists of four questions that help medical professionals evaluate a patient's mental health. Its purpose is to screen for anxiety and depression symptoms and determine if further evaluation or treatment is necessary.
This type of document provides structured formats to create tailored plans for individuals undergoing art therapy. It helps therapists in outlining goals, treatment methods, and progress tracking.
This document is a sample treatment plan that outlines the proposed course of action for managing a patient's medical condition. It includes details such as recommended treatments, medications, and follow-up procedures.
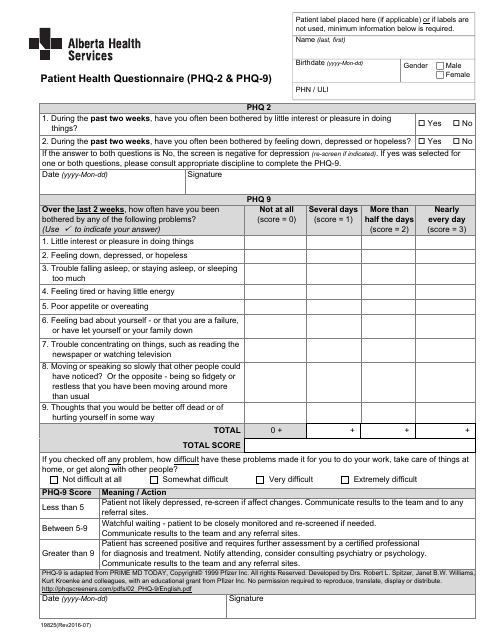
This document is a form used by Pfizer Inc. for assessing a patient's mental health. It is known as the Patient Health Questionnaire (PHQ-9).
This document is a questionnaire used to assess a patient's mental health. It measures the severity of depression symptoms and helps healthcare providers determine appropriate treatment options.
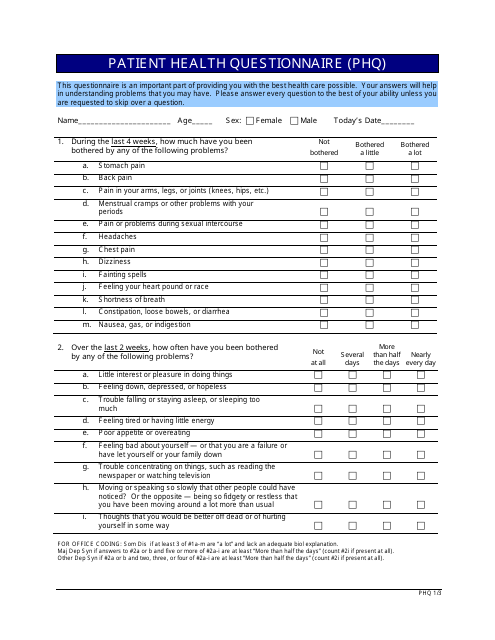
This form is used for assessing a patient's mental health and screening for common mental disorders such as depression and anxiety. The Patient Health Questionnaire (PHQ) helps healthcare providers gather information about a patient's symptoms and make an accurate diagnosis.
This type of document provides a score report for the PHQ-9 assessment, which is commonly used to screen for depression.
This form is used by healthcare practitioners in Alberta, Canada to screen patients for depression by utilizing the PHQ-2 and PHQ-9 tools, which measure the symptoms and severity of depression.
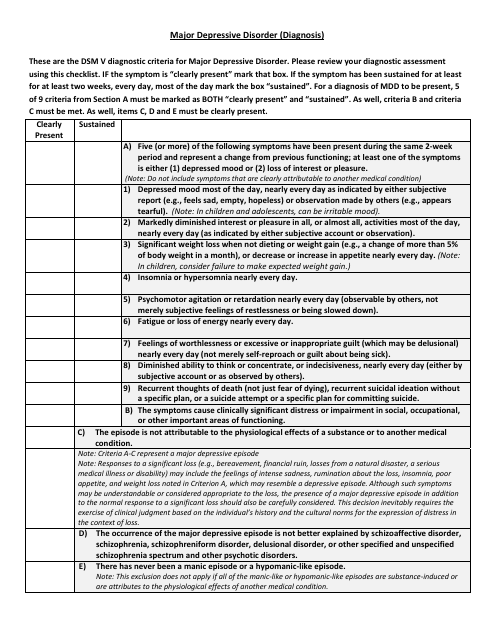
This type of document provides comprehensive details on how Major Depressive Disorder is identified and diagnosed, including possible symptoms, differential diagnoses, and assessment tools utilized in clinical settings.
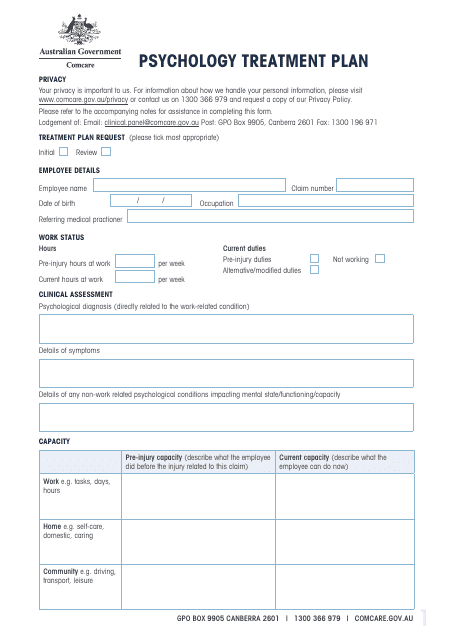
This document outlines a comprehensive, personalized approach to improving mental health, specifically for those living in Australia. It details strategies for treatment, goals to be achieved, and a timeline for progress.
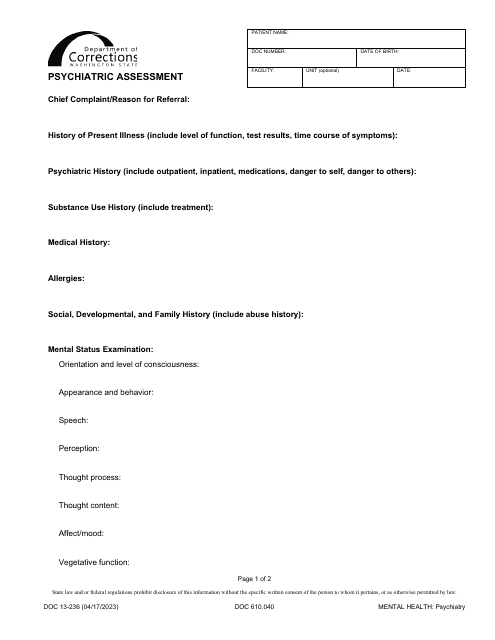
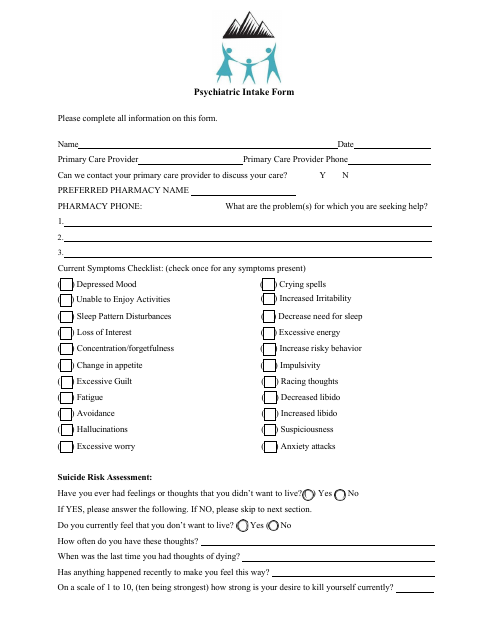
This form is used by healthcare professionals to gather comprehensive information about a new patient's mental health history and current mental state. It assists in diagnosing potential psychiatric disorders and formulating a suitable treatment plan.
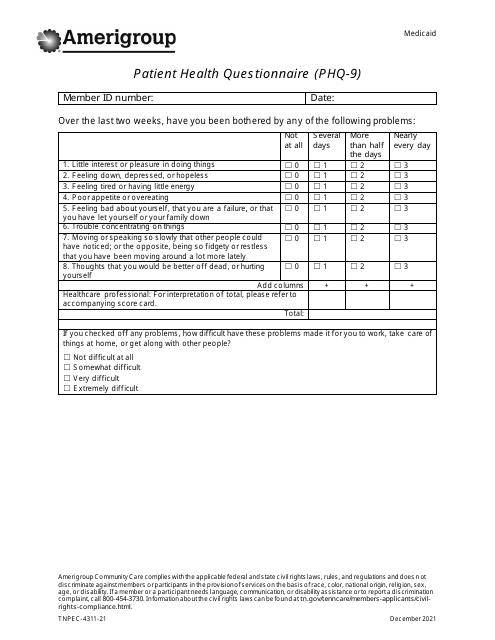
This document is a screening tool utilized by Amerigroup to gauge the severity of a patient's depression. It aids healthcare professionals in understanding the patient's mental health status for proper diagnosis and treatment.
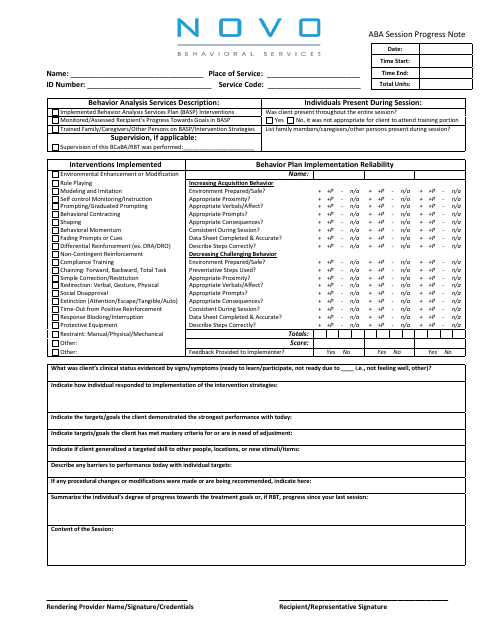
This document is a tool utilized by Novo Behavioral Services to record the progress and updates of individuals undergoing Applied Behavior Analysis sessions. It notes observations, treatment insights and the future course of action.
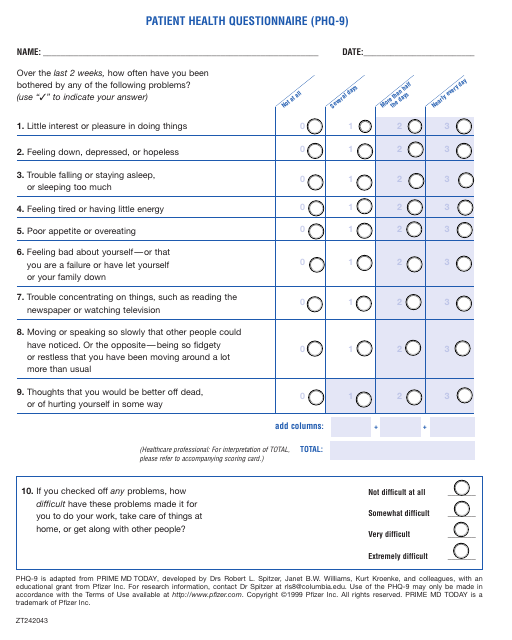
This document is a Patient Health Questionnaire (PHQ-9) created by Pfizer. It is used to assess and monitor a patient's mental health by asking questions about their mood, energy levels, and other symptoms related to depression. The PHQ-9 is commonly used by healthcare professionals to help diagnose and treat depression.
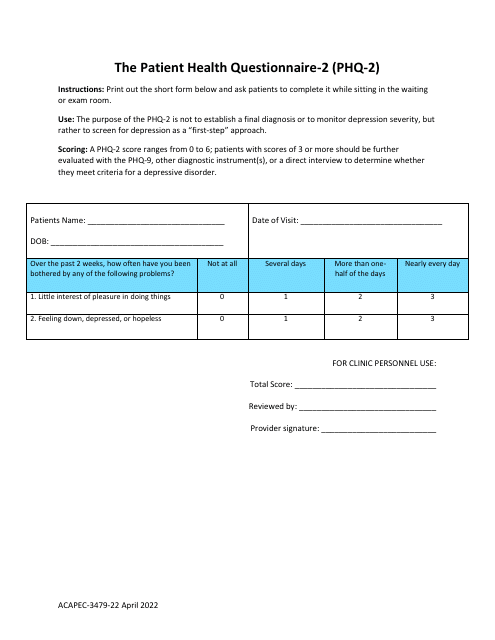
This form is used for initial screening of patients for possible depression, consisting of two simple questions to gauge mental health status. It plays a crucial role in identifying symptoms and pointing towards necessary psychiatric intervention.
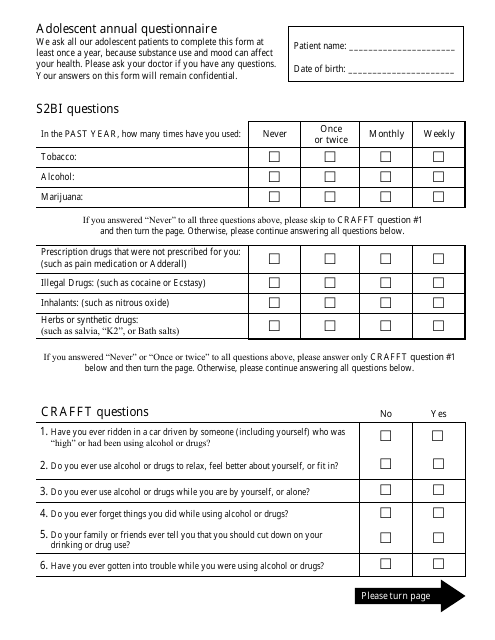
This document is utilized to track and record health information and changes in adolescent individuals annually. The information obtained aids in providing comprehensive medical care for the adolescent patient.